Introduction
Emerging evidence supports telepractice as a service model with great clinical potential. From live videoconferencing to asynchronous interactive programs, to remote monitoring systems and web-based educational support services, all have capacity to help enhance dysphagia management. The following summary highlights the current evidence for a range of different telepractice models and their applications for dysphagia management. For readers interested in this area, additional recent summary articles are also provided as references for further reading.
Screening and Clinical assessment
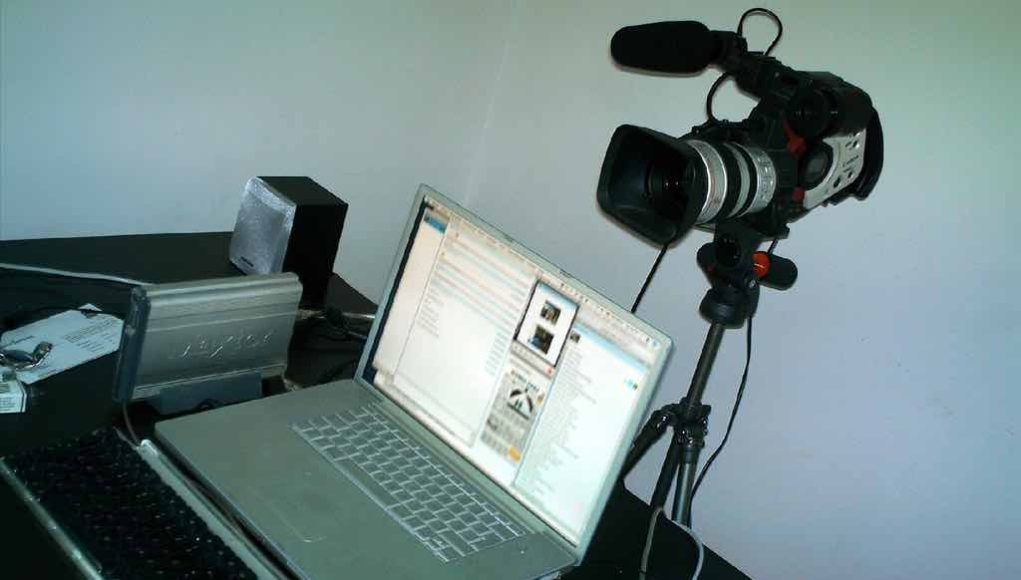
A series of studies conducted by Ward and colleagues has demonstrated initial viability and clinical equivalence of conducting a clinical swallowing examination (CSE) via telepractice1-6. This model enables clinicians to screen patients for dysphagia risk, review status and triage management options for patients unable to access face to face services. Using live videoconferencing over a secure health service network, the model requires specific equipment set up (eg., adequate lighting, free standing speakers and lapel microphones, fixed and free standing webcameras) and other key modifications to the procedure (eg., use of clear utensils to enable view of delivery of the bolus, volumes consumed and residue; a tape marker at level of thyroid cartilage to enhance view of laryngeal movement)1-3. The service model also involves a trained assistant7 at the patient end, to assist trials under direction of the online clinician and to ensure patient safety in an emergency situation. Patient satisfaction with the model is reported as high6. Conducting a CSE to determine best functional diet consistencies for patients post laryngectomy has also been described8,9.
Use of asynchronous models to screen patient issues, including dysphagia, are also being trialled with patients undergoing head and neck cancer (HNC) management10,11. A project by Wall et al is using asynchronous computer based screening models to enable patients attending (chemo)radiotherapy to self-report current treatment toxicities, dysphagia symptoms and mealtime issues on a routine basis during treatment11. This information is then accessed by their managing clinician to identify priority areas for management and assist referral for additional services. A parallel system has also been designed for the carers of patients undergoing HNC management11. In recognition of the significant negative impacts carers can experience when supporting someone with oral intake issues, this simple screening system asks carers to indicate the extent and nature of both general and any mealtime related distress. Information can then be accessed by the patients’ managing clinician, to ensure the carer is also receiving timely and appropriate management/referral for these issues.
Instrumental Assessment
An emerging body of research has also investigated the application of telepractice in instrumental swallowing assessments12-16. The Teledynamic Software System (TESS) was the first system to describe the transmission of videofluroscopic swallow study (VFSS) images over the internet12. This configuration involved a computer based system transmitting live x-ray images from the fluoroscopy suite to a remote location. The clinical application of TESS was subsequently tested by Malandraki and colleagues with 32 adults with dysphagia13. An innovative study of its time, it demonstrated the potential for telefluoroscopy. However the authors acknowledged that inconsistencies in data transmission impacted on the clinician’s ability to accurately interpret the live VFSS images. With technological advances, there has been greater capacity to enhance telepractice systems to support live fluoroscopic image transmission. Burns et al.15 reported that image quality during live transmission could be preserved using higher bandwidths over a range of telepractice system configurations. The clinical feasibility of this system was recently tested by Burns et al16 in a simulated trial with a small group of dysphagic patients and results will be available in press shortly. Results demonstrated the system enabled remote direction and real time interpretation of the VFSS study supporting the potential for the development of real-time VFSS telepractice services16.
Preliminary reports have described the nasendoscopy assessment via telepractice17,18, however no studies to date have incorporated Fibreoptic Endoscopic Evaluation of Swallowing (FEES). Burns et al have trials currently underway exploring image quality transmission and cohort trials, with results expected late 2016. Future studies evaluating both the technical and clinical aspects of tele-endoscopy are required to ensure both the clinical procedure and remote image quality enables accurate assessment and diagnosis.
Management
Whilst applications of telepractice for dysphagia therapy are still in their infancy, recent research with HNC patients has shown great promise. A pilot study by Burns et al19 described a telepractice system using live videoconferencing to conduct dysphagia and laryngectomy management without needing patients to travel long distances to tertiary centres. There is also the potential for asynchronous telepractice systems (using “store and forward” technology) to further benefit both patients and clinicians – allowing patients to complete dysphagia therapy in their homes and clinicians to interact and review progress remotely20. However, it is important to ensure that these systems are developed with patients’ needs in mind and that they feel supported to direct their dysphagia therapy independently, without real-time clinician input. A recent pilot study by Wall et al evaluated HNC patient perceptions of a new asynchronous telepractice application, “SwallowIT”, to deliver intensive, preventative swallowing therapy during treatment20. Patients reported high levels of comfort, confidence, support and motivation to complete their dysphagia therapy using SwallowIT – a purpose-built application which uses instructional videos, text and interactive messaging with the clinician. The team has further research underway comparing the equivalence of clinical swallowing outcomes achieved via SwallowIT, versus traditional face-to-face services.
Client Handover, Clinical Support and Mentoring
Telepractice holds great potential to enhance workforce capabilities14,19, 21. Various different telepractice models can be used in this context. Live videoconferencing can facilitate interactions between clinicians and provide opportunities for clinical up-skilling. In their pilot study of a telepractice model for post discharge support for clients with HNC, including dysphagia management, Burns et al19 discussed the use of live videoconferencing to enable the experienced clinician to assist the local, less experienced clinician “complete necessary clinical tasks safely and effectively” (p 446). The use of asynchronous telepractice models to provide expert consultation has also been reported. Malandraki et al.14 described transferring (via the web) VFSS studies from a hospital in Greece to a specialist clinician in the USA for analysis. Discrepancies in decision making between the local novice clinician and the expert remote clinician highlighted the positive potential for teleconsultation models to support novice clinicians with VFSS interpretation and treatment planning.
Where to from here?
Although the evidence in this field is emerging, the scope for further research and development is enormous. As for all new models of care, systematic validation of efficacy, safety, cost efficiency, and consumer (patient, and services) satisfaction is needed for all new telepractice applications. Evaluation of full scale clinical translation of telepractice models is also required. The evidence available to date, however, highlights the great potential for telepractice to become an integral component of dysphagia management practices in the future.
Suggested additional reading
- Ward E.C. & Burns, C. (2014) Dysphagia Management via Telerehabilitation: A review of the current evidence. Journal of Gastroenterology and Hepatology Research. 3(5), 1088-1094
- Burns, C., Hill, A., & Ward, E.C (2014). Supporting head and neck cancer management: Use of technology. In E.C. Ward & C.J. van As-Brooks (Eds.). Head and neck cancer: Treatment, rehabilitation and outcomes 2nd Edition (p 541-568). San Diego, USA: Plural Publishing.
Contributing Authors
Elizabeth (Liz) Ward. Liz is the Professor of the Centre for Functioning and Health Research (CFAHR) within Queensland Health and a conjoint Professor at The University of Queensland, Australia. She is an experienced clinical researcher with over 200 publications across the research areas of telepractice and the rehabilitation of speech and swallowing disorders in a range of clinical populations including head and neck cancer, critical care and degenerative disorders. Details of her publications and current projects can be found at http://researchers.uq.edu.au/researcher/304
Clare Burns. Clare is an advanced speech pathologist at the Royal Brisbane & Women’s Hospital, Australia. She specialises in the area of head and neck cancer and instrumental swallowing assessment and over the last 5 years has lead clinical research and implementation of telepractice speech pathology services within Queensland, Australia. She is currently undertaking her PhD evaluating the application of telepractice in the swallowing and communication management of patients following head and neck cancer treatment.
Laurelie Wall. Laurelie is a PhD candidate with the Centre for Functioning & Health Research (CFAHR) and The University of Queensland, Australia. She also works clinically as an acute-care speech pathologist at the Princess Alexandra Hospital in Brisbane, Australia. Her PhD focuses on the use of technology-assisted service-delivery models to enhance aspects of dysphagia assessment and management with head and neck cancer patients. http://www.researchgate.net/profile/Laurelie_Wall.
References
- Sharma, S., Ward, E. C., Burns, C., Theodoros, D. G., & Russell, T. (2011) Assessing swallowing disorders online: a pilot telerehabilitation study. Journal of Telemedicine and e-Health, 17(9), 688-695.
- Ward, E. C., Sharma, S., Burns, C., Theodoros, D. G., & Russell, T. (2012). Validity of conducting clinical dysphagia assessments with patients with normal to mild cognitive impairments via telerehabilitation. Dysphagia, 27(4), 460-472.
- Ward E.C, Burns, C., Theodoros, DG, & Russell, T (2014). Impact of dysphagia severity on clinical decision making via telerehabilitation. Telemedicine and e-Health. 20(4), 296-303.
- Ward E. C., Burns, C., Theodoros, D. G., & Russell, T. (2013). Evaluation of a Clinical Service Model for Dysphagia Assessment via Telerehabilitation,” International Journal of Telemedicine and Applications, vol. 2013, Article ID 918526, 7 pages, 2013.
- Ward, E. C., Sharma, S., Burns, C., Theodoros, D. G., & Russell, T. (2012). Managing patient factors in the assessment of swallowing via telerehabilitation. International Journal of Telemedicine and Applications, 1-6.
- Sharma, S., Ward, E. C., Burns, C., Theodoros, D. G., & Russell, T. (2013). Assessing dysphagia via telerehabilitation: Patient perceptions and satisfaction. International Journal of Speech-Language Pathology, 15(2), 176-183.
- Sharma, S., Ward, E C., Burns, C., Theodoros, D G., & Russell, T. (2012) Training the allied health assistant for the telerehabilitation assessment of dysphagia. Journal of Telemedicine and Telecare, 18, 287-291.
- Ward, E., Crombie, J., Trickey, M., Hill, A., Theodoros, D., & Russell, T. (2009). Assessment of communication and swallowing post-laryngectomy: a telerehabilitation trial. Journal of Telemedicine and Telecare, 15(5), 232-237.
- Ward, E., White, J., Russell, T., Theodoros, D., Kuhl, M., Nelson, K., & Peters, I. (2007). Assessment of communication and swallowing function post laryngectomy: a telerehabilitation trial, Journal of Telemedicine and Telecare, 3(3), 88-91.
- Wall L. R., Ward E. C., Cartmill B., Hill A. J. (2013) Technology-assisted screening of patient-reported functional outcomes in the head and neck cancer population: What’s the evidence? OA Cancer, Oct 01;1(2):13
- Wall, L., Ward, E., Cartmill, B., Hill, A., Isenring, E., Byrnes, J., Chambers, S., Dunn, J., Nixon, J., Whelan, J., Porceddu, S. (2015). Computerised screening of swallowing, nutrition and distress in head and neck cancer patients and their carers. Dysphagia, 30(5), 667-667.
- Perlman, A. L., & Witthawaskul, W. (2002). Real-time remote telefluoroscopic assessment of patients with dysphagia. Dysphagia, 17(2), 162-167.
- Malandraki, G. A., McCullough, G., He, X., McWeeny, E., & Perlman, A. L. (2011). Teledynamic evaluation of oropharyngeal swallowing. Journal of Speech Language and Hearing Research, 54(6), 1497-1505.
- Malandraki, G. A., Markaki, V., Georgopoulous, V. C., Bauer, J. L., Kalogeropoulos, I., Nanas, S. (2013). An international pilot study of asynchronous teleconsultation for oropharyngeal dysphagia. Journal of Telemedicine and Telecare, 19, 75-79.
- Burns, C. L., Keir, B., Ward E. C., Hill, A. J., Farrell, A, Phillips, N., Porter, L (2015). A dynamic image quality evaluation of videofluoroscopy images: Considerations for telehealth applications. 30(4), 473-481.
- Burns, C. L., Ward E. C. , Hill, A. J., Phillips, N., Porter, L. (under review) Conducting real-time videofluoroscopic swallow study via telepractice: A feasibility study.
- Dorrian C, Ferguson J, et al. (2009). Head and neck cancer assessment by flexible endoscopy and telemedicine. Journal of Telemedicine and Telecare, 15, 118-21.
- Burns, C. L., Ward, E. C., Hill, A. J., Malcolm, K., Bassett, L., Kenny, L. M., Greenup, P. (2012). A pilot trial of a speech pathology telehealth service for head and neck cancer patients. Journal of Telehealth and Telecare, 18(8), 443-446.
- Wall, L. R., Ward, EC, Cartmill, B., Hill, A. J., & Porceddu, S. V. (In press). Examining user perceptions of “SwallowIT”: A pilot study of a new telepractice application for delivering intensive swallowing therapy to head and neck cancer patients. Journal of Telehealth and Telecare.
- Coyle, J. (2012). Tele-dysphagia management: An opportunity for prevention cost-savings and advanced training. International Journal of Telerehabilitation, 4(1), 37-4.