Aphasia to dysphagia
It is sometimes hard to fathom that I saw my first dysphagia case 37 years ago! In 1980 I was a consultant at a local VAMC while teaching at a university in the Midwest. I was seeing a lot of patients with aphasia.
Recognize where we came from, embrace it, but push forward to learn from and work with many other professions toward the betterment of our patients.
One day the chief of neurology approached me about seeing a patient. “What type of aphasia does he have?” I queried. “None” responded the neurologist – he has trouble swallowing. Like many of my generation I had just heard Dr. Logemann present at the state convention on her early work in this area. So I took on the case and if memory serves I was able to provide help! (Or perhaps the patient recovered despite my intervention!)
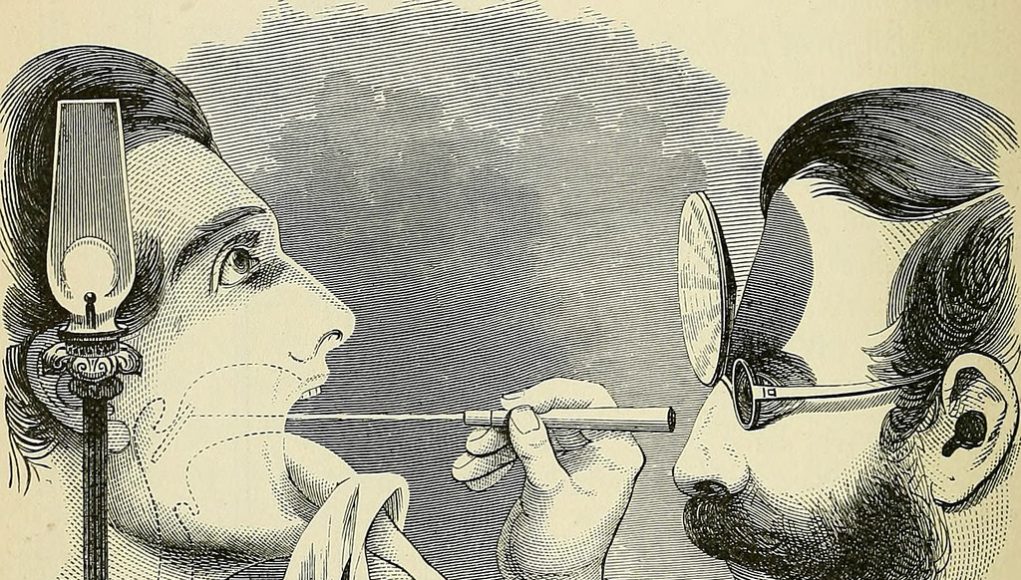
Laryngeal mirrors and beyond
What has become interesting to me is the ongoing change in how we assess and treat patients with swallowing disorders. As a young clinician I carried a cup of ice in one pocket and a bunch of small laryngeal mirrors in another. Why…it is what we were taught to do! And, we rarely looked lower than the PES (we called it UES in those days!) during fluoroscopic swallowing evaluations. Today we have standardized and validated clinical tools to evaluate swallowing problems, we have multiple treatment options to apply to various problems – each with some degree of supportive evidence. We have adjunctive modalities and are learning more and more how to use them properly. Moreover, we enjoy a degree of interprofessional collaboration that we did not even think of in those early days, working with physicians, engineers, corporate partners, and more. We now have opportunities to learn not only about new tools, but how to use these tools to assess pH levels in the pharynx and esophagus, swallowing pressures and bolus flow in these same regions, advanced brain imaging strategies, and more.
Practicing in exciting times
I have given up explaining to my students what it was like in those early days – they will never have those experiences.
Dr Crary is associated with the Florida Dysphagia Institute version 2.0 (FDI 2.0). For more information please go to https://www.fdi2.org/
But, what excites me the most is that this niche interprofessional area continues to grow rapidly. Recently, we witnessed the launching of the first interprofessional degree program in ‘deglutology’ by Dr Nathalie Rommel and her colleagues at the University of Leuven in Belgium. We are seeing more and more technical advances that might be of help in evaluating and/or treating patients with swallowing difficulties. Speech-Language Pathologists are working side by side with a variety of medical colleagues and actively participating in new and wonderful techniques that were not available a few short years ago. We are learning about treatment approaches that can rehabilitate patients with severe dysphagia in a few weeks. These are exciting times.
Challenge for future clinicians
In the end, my message is to keep learning – keep challenging the status quo – foster new discoveries – share your information and your opinions openly and be open to other points of view and other pieces of information. Engage in opportunities to keep moving forward. I am not ready to hang up my laryngeal mirrors or my HRM catheters. However, I do want to challenge those clinicians and researchers who have followed a brief but productive path blazed by those who I considered pioneers. Recognize where we came from, embrace it, but push forward to learn from and work with many other professions toward the betterment of our patients. To quote a former cigarette ad – ‘we’ve come a long way baby’ – and we have much farther to go. Only by standing on the shoulders of giants can we see the future more clearly. I pay homage to those who taught me formally and informally and I challenge those who are forging the future to do the same.
Links of interest
- Dr Crary is associated with the Florida Dysphagia Institute version 2.0 (FDI 2.0). The inaugural event for FDI 2.0 will be a week long course in Orlando, FL from July 10 – 14, 2017. For more information please go to https://www.fdi2.org/