Co-Author: Georgia A. Malandraki, PhD, CCC-SLP, BCS-S
Introduction
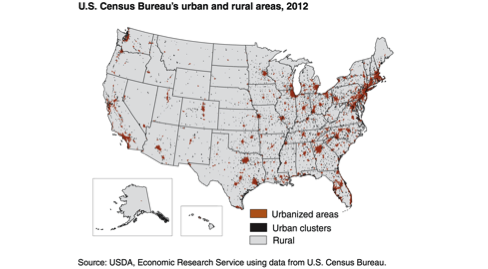
The dramatic changes in the way we use technology have helped us tackle many long-standing problems, including the provision of high-quality healthcare services to all individuals irrespective of where they live. Although most people who live in urban areas receive health services without experiencing major interruptions in their daily lives, the opposite is true for 59 million Americans who live in rural areas of the country (Figure 1).[1] Due to this fact, these people often experience poorer health outcomes.[1] Stemming from a need to make healthcare services more accessible and to provide the same quality of care to all, telehealth has emerged as a feasible alternative to conventional service delivery approaches. The term “telehealth” is applied to any area of healthcare where technology is employed in the evaluation, diagnosis, treatment, or monitoring of medical conditions remotely.

Over the last few decades, telehealth has been gaining momentum in research and clinical practice in a wide variety of disciplines, including speech-language pathology and dysphagia management. Specifically, there is gradually accumulating research evidence to support the use of telehealth in the management of dysphagia.[2-13] This evidence was reviewed on Dysphagia Café by Ward et al. in December and is beyond the scope of this article. Our aim is to review the benefits and limitations of telehealth as they relate to dysphagia management, discuss the current state of dysphagia telehealth in the United States, and provide information on the next steps needed to advance the remote management of dysphagia in the US.
Benefits of telehealth for dysphagia management
It is undeniable that telehealth has remarkable benefits to offer. Improved access to care, reduced healthcare costs, and decreased wait and travel times are commonly reported. [14-15] In addition, it has been shown that telehealth can increase treatment compliance, improve health outcomes due to delivery of timely and high-quality services from specialists, [14-15] and facilitate remote consultations between clinicians [3,16-18]
Patients with dysphagia who live in rural, remote, and underserved areas or who have mobility limitations experience difficulty in accessing quality healthcare services and medical experts, including clinicians who specialize in dysphagia.[17-18] These challenges often result from the limited number of dysphagia experts available in rural areas, or from lack of physical resources necessary for dysphagia related services.[17-18] For example, rural hospitals might not have the necessary radiologic equipment to conduct Videofluoroscopic Swallow Studies (VFSS), nor an expert dysphagia specialist who can adequately diagnose and treat swallowing difficulties. In addition, when patients have to travel long distances to go to the nearest hospital, they may be physically tired by the time of the appointment, and clinicians may not get a good representation of their patients’ swallowing skills. Due to the potentially life-threatening consequences of dysphagia, timely and accurate evaluation and treatment of swallowing function is absolutely crucial.[19] Telehealth has the potential to meet this critical need and warrants our continued clinical and research efforts.
Current challenges in dysphagia telerehabilitation in the United States
Despite all the benefits, and the growing interest for telehealth among speech-language pathologists, its use in dysphagia management has been limited in the US and globally. The reasons for this slow adoption are multifaceted and include policy and legal issues, practical aspects of service delivery, and slow accumulation of empirical evidence.
Telehealth, once a novel approach, is currently gaining momentum as a mode of healthcare service delivery because of its potential in diminishing inequalities and improving access to care.
Policy and legal issues involve the challenges with licensing and reimbursement. State licensures continue to restrict clinicians to provide services to individuals within the same state, therefore significantly limiting the geographic borders of telehealth services.[20] Regarding reimbursement, although Medicaid, Medicare Part B, and private insurance agencies provide some coverage for telehealth services delivered by speech-language pathologists (SLPs), currently there are many restrictions for the types of telehealth services that can be reimbursed.[21] For example, in some states, school-based telehealth services are the only type of services covered; in other states live videoconferencing, where the clinicians and the patients interact in real-time, is required for reimbursement.[21] Similarly, 29 states require that private insurance agencies provide similar coverage for telehealth services compared to the in-person services, but many other states still impose restrictions.[21] These reimbursement limitations currently restrict the growth of telehealth in our field.[18] Finally, liability insurance coverage for telehealth malpractice is not included in most of the current liability insurance plans and/or is an add-on expense for many healthcare providers.[22]
Practical challenges specific to dysphagia further complicate the use and adoption of telehealth for dysphagia clinicians. Specifically, providing high quality dysphagia services from a distance necessitates the assurance of a number of diagnostic parameters, such as excellent video and audio quality, high speed transmission of the signal to ensure real-time viewing of the patient/diagnostic modality, as well as accurate remote monitoring of physiological signs of distress (e.g., signs of aspiration/penetration, respiratory and cardiac rate etc.). Furthermore, lack of physical proximity can be limiting, as it makes it more difficult to share documents, carry on hands-on tasks, such as the 4-finger palpation, and train patients on completing exercises. To overcome these challenges, appropriate training and mentorship, as well as acquisition of the right equipment is needed, and these are not frequently or widely available.
Regarding research evidence, as reviewed by Ward et al. there are a number of studies that have examined the feasibility, reliability, and effectiveness of telehealth in dysphagia management. [2-13] Most of these studies provide positive and encouraging outcomes, but have been mainly diagnostic, focusing largely on adult patients, and have used specialized or custom-made equipment that are not widely available. Regarding providing dysphagia treatment from a distance, research evidence only includes one case study[5] and small-scale satisfaction surveys on the use of dysphagia apps.[12] Therefore, it is clear that, in addition to overcoming the previously discussed policy, legal and practical issues, significant continued research efforts are also needed before this new service delivery model can be widely adopted in clinical practice.
Potential solutions and next steps
In this section, we discuss potential solutions to the aforementioned challenges. As reported earlier, currently SLPs can only provide telehealth services to in-state patients.[23] Although it is also challenging for physicians to practice medicine across state lines, there have been recent developments in the medical field that may spearhead improvements for allied health professions. Specifically, several states allow licensure reciprocity to physicians from neighboring states, and in some states special licenses for out-of-state physicians are offered.[20] It is our belief that as telehealth becomes more mainstream, licensing restrictions for our field will also decrease. Reimbursement for telehealth services is also increasing slowly but steadily.
Currently, there are many pending bills at the state and federal levels in line to be reviewed. Organizations, such as the American Telemedicine Association (ATA) and the American Speech-Language and Hearing Association (ASHA), are actively advocating for less restrictions on reimbursement. For example, ASHA has recently endorsed a bill that aims to improve Medicare coverage for telehealth services provided by SLPs.[24] It is only a matter of time that reimbursement issues for telehealth services will be resolved. In the meantime, clinicians interested in this area need to contact their state Medicare and Medicaid representatives, as well as their state associations, to inquire about the exact reimbursement coverage and restrictions for services in their state before initiating any telehealth efforts. In addition, SLPs should be aware of the risks involved in telehealth service provision (including risks of confidentiality and data breach) and ensure that their liability insurance covers telehealth related services in the states they serve. Finally, having legal counsel involved in telehealth efforts cannot be overemphasized. State and federal telehealth laws change almost monthly; the expertise of a specialized legal counselor who can stay abreast of all these updates and changes can be invaluable.
Once adopted, [telehealth] has the potential to make quality dysphagia management what it should be, not a privilege, but a right for everyone.
To overcome some of the practical challenges, telehealth programs should invest in high quality, HIPAA-aligned equipment and software, as well as in encrypted and high-speed Internet services that comply with all relevant laws and regulations for technical safety.[25] Consulting and collaborating with an IT specialist would be particularly important for becoming familiar with safety issues and finding solutions to potential problems. Dysphagia clinicians could also benefit from remote patient monitoring devices such as remotely controlled pulse oximeters and digital scales to keep track of basic vital signs and weight loss, and high quality and portable peripheral cameras with zoom in function to closely and adequately examine head and neck structures. As mentioned earlier, lack of physical proximity can be especially challenging when delivering dysphagia services. In addition to the steps described above, studies have shown that having a trained assistant in the room with the patient can be very helpful in overcoming some of these challenges.[26]
Lastly, although the research evidence on the use of telehealth for dysphagia management has shown positive results, as of today there are no randomized controlled trials that have been conducted to examine the use of telehealth in dysphagia management. Furthermore, more research is needed in order to increase generalization in more patient populations, and to assess all evaluation modalities (including Fiberoptic Endoscopic Evaluation of Swallowing), and interventions. The use of remote patient monitoring devices and wearable sensors that are frequently used by physicians practicing telemedicine should also be investigated in our field, as their use could be important in enabling adequate remote patient monitoring. Finally, we are well aware that high quality research takes time and requires financial resources that are not always available. In the US, there are private and government agencies (e.g., NIH, U.S. Department of Agriculture) that offer grants to research institutes and programs that serve people who live in rural and underserved areas of the country. Applying for these grants can provide funding necessary for conducting more studies in dysphagia telehealth.
Conclusions
The majority of allied health professionals, including speech-language pathologists, work in urban areas. Yet, rural areas occupy the 95% of the landmass of the United States (Figure 2). Given the limited number of dysphagia experts in these areas, it is evident that we need to find more ways to serve patients that live in rural areas or have significant mobility restrictions. Telehealth, once a novel approach, is currently gaining momentum as a mode of healthcare service delivery because of its potential in diminishing inequalities and improving access to care. It is the belief of these authors that with the recent developments in telehealth, the current aforementioned challenges will soon be resolved and telehealth services will be more widely available. It is important to emphasize, however, that for the use of telehealth to be effective and ethical, no regulatory distinction should exist between a service delivered face-to-face and a service delivered via telehealth. Thus, it is evident that much more research is needed before telehealth can be widely used for dysphagia services. Once adopted, it has the potential to make quality dysphagia management what it should be, not a privilege, but a right for everyone.
Links of Interest
- Purdue University I-Eat Research Lab
- American Telemedicine Association
- ASHA’s Practice Portal on Telepractice
- Telehealth Resource Center
- Center for Telehealth and e-Health Law
- International Society for Telemedicine and e-Health
- Telemedicine and e-Health Information Service
About the Authors
Cagla Kantarcigil, MS, SLP is a doctoral student in the Dept. of Speech, Language, & Hearing Sciences at Purdue University. She is also a research assistant in the Purdue I-EaT (Imaging, Evaluation, & Treatment of Swallowing) Swallowing Research Laboratory. Her research interests include investigating the effectiveness of telehealth in the assessment and treatment of dysphagia.
Georgia A. Malandraki, PhD, CCC-SLP, BCS-S is an Assistant Professor in the Dept. of Speech, Language and Hearing Sciences at Purdue University and a Board Certified Specialist in Swallowing and Swallowing Disorders. She is also the Research Director of the Purdue I-EaT Swallowing Research Laboratory and Clinic. Her research focuses on: a) the use of imaging and neuro-imaging to understand the neuroplastic properties of the brain in pediatric and adult dysphagia; b) developing new intensive neurorehabilitation paradigms and examining their effectiveness for neurogenic dysphagia; and, c) the development of valid and reliable teledynamic systems to test the effectiveness of providing swallowing management over the Internet.
References
- Hartley, D. (2004). Rural health disparities, population health, and rural culture. American Journal of Public Health, 94(10), 1675-1678.
- Burns, C. L., Ward, E. C., Hill, A. J., Phillips, N., & Porter, L. (2016). Conducting real-time videofluoroscopic swallow study via telepractice: a preliminary feasibility and reliability study. Dysphagia, 1-11.
- Malandraki, G. A., Markaki, V., Georgopoulos, V. C., Bauer, J. L., Kalogeropoulos, I., & Nanas, S. (2013). An international pilot study of asynchronous teleconsultation for oropharyngeal dysphagia. Journal of Telemedicine and Telecare, 19(2), 75-79.
- Malandraki, G. A., McCullough, G., He, X., McWeeny, E., & Perlman, A. L. (2011). Teledynamic evaluation of oropharyngeal swallowing. Journal of Speech, Language, and Hearing Research, 54(6), 1497-1505.
- Malandraki, G. A., Roth, M., & Sheppard, J. J. (2014). Telepractice for Pediatric Dysphagia: A Case Study. International Journal of Telerehabilitation, 6(1), 3-16.
- Sharma, S., Ward, E. C., Burns, C., Theodoros, D., & Russell, T. (2013). Assessing dysphagia via telerehabilitation: patient perceptions and satisfaction. International Journal of Speech-language Pathology, 15(2), 176-183.
- Sharma, S., Ward, E. C., Burns, C., Theodoros, D., & Russell, T. (2011). Assessing swallowing disorders online: a pilot telerehabilitation study. Telemedicine and E-Health, 17(9), 688-695.
- Wall, L. R., Cartmill, B., Ward, E. C., Hill, A. J., Isenring, E., Byrnes, J., … & Porceddu, S. V. (2016). “ScreenIT”: Computerized screening of swallowing, nutrition and distress in head and neck cancer patients during (chemo) radiotherapy. Oral Oncology, 54, 47-53.
- Ward, E. C., Burns, C. L., Theodoros, D. G., & Russell, T. G. (2013). Evaluation of a clinical service model for dysphagia assessment via telerehabilitation. International Journal of Telemedicine and Applications,1-7.
- Ward, E. C., Sharma, S., Burns, C., Theodoros, D., & Russell, T. (2012). Validity of conducting clinical dysphagia assessments for patients with normal to mild cognitive impairment via telerehabilitation. Dysphagia, 27(4), 460-472.
- Ward, E. C., Burns, C. L., Theodoros, D. G., & Russell, T. G. (2014). Impact of dysphagia severity on clinical decision making via telerehabilitation. Telemedicine and E-Health, 20(4), 296-303.
- Wall, L. R., Ward, E. C., Cartmill, B., Hill, A. J., & Porceddu, S. V. (2015). Examining user perceptions of SwallowIT: a pilot study of a new telepractice application for delivering intensive swallowing therapy to head and neck cancer patients. Journal of Telemedicine and Telecare.
- Kantarcigil, C., Sheppard, J. J., Gordon, A. M., Friel, K. M., & Malandraki, G. A. (2016). A telehealth approach to conducting clinical swallowing evaluations in children with cerebral palsy. Research in Developmental Disabilities, 55, 207-217.
- Jennett, P. A., Hall, L. A., Hailey, D., Ohinmaa, A., Anderson, C., Thomas, R., … & Scott, R. E. (2003). The socio-economic impact of telehealth: a systematic review. Journal of Telemedicine and Telecare, 9(6), 311-320.
- Wade, V. A., Karnon, J., Elshaug, A. G., & Hiller, J. E. (2010). A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Services Research, 10(1), 233.
- Ferguson, J. (2006). How to do a telemedical consultation. Journal of Telemedicine and Telecare, 12(5), 220-227.
- Coyle, J. (2012). Tele-dysphagia management: An opportunity for prevention, cost-savings and advanced training. International Journal of Telerehabilitation, 4(1), 37.
- Ward, E. C., & Burns, C. L. (2014). Dysphagia management via telerehabilitation: a review of the current evidence. Journal of Gastroenterology and Hepatology Research, 3(5).
- Malandraki & Robbins (2013). Dysphagia. In M. P. Barnes & D. C. Good (Eds.), Neurological Rehabilitation, Volume 110: Handbook of Clinical Neurology (255-271). Elsevier.
- Thomas, L., & Capistrant, G. (2016, January). State telemedicine gaps analysis: physician practice standards & licensure. Retrieved from http://www.americantelemed.org/docs/default-source/policy/2016_50-state-telehealth-gaps-analysis-md-physician-practices-licensure.pdf?sfvrsn=2
- Thomas, L., & Capistrant, G. (2016, January). State telemedicine gaps analysis: coverage & reimbursement. Retrieved from http://www.americantelemed.org/docs/default-source/policy/2016_50-state-telehealth-gaps-analysis–coverage-and-reimbursement.pdf?sfvrsn=2
- Stanberry, B. (2006). Legal and ethical aspects of telemedicine.Journal of Telemedicine and Telecare, 12(4), 166-175.
- American Speech, Language, and Hearing Association. (n.d.). Telepractice practice portal. Retrieved from http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934956§ion=Key_Issues#Licensure_and_Teacher_Certification
- American Speech, Language, and Hearing Association. (2016). Medicare telehealth coverage for audiology and speech, language pathology services. Retrieved from http://www.asha.org/uploadedFiles/IB-Medicare-Telepractice-Coverage-AUD-SLP-Services.pdf
- American Telemedicine Association (2010, October). A blueprint for telerehabilitation guidelines. Retrieved from http://www.americantelemed.org/docs/default-source/standards/a-blueprint-for-telerehabilitation-guidelines.pdf?sfvrsn=4
- Sharma, S., Ward, E. C., Burns, C., Theodoros, D., & Russell, T. (2012). Training the allied health assistant for the telerehabilitation assessment of dysphagia. Journal of Telemedicine and Telecare, 18(5), 287-291.





