Let’s Talk IDDSI
Recently members of our team attended the Leading Age conference in Minnesota. This gathering of professionals provided us an opportunity to speak with several service providers who work in the field of aging. These conversations quickly became discussions focused on transitional foods, finger foods and implementation of the International Dysphagia Diet Standardization Initiative (IDDSI).
When you conduct an internet search for “transitional food”, you often find articles discussing transitioning babies and toddlers from purees to solids. You may also find sources that describe the process of converting conventional agricultural products to organic (Source: Shape.com, Sept 26, 2016) or changing from one customary way of eating food to another like cooked vs. raw (Source: Homegrownandhealthy.com, Feb 5, 2013). If you add the word “dysphagia” to your search, you will often be directed to the IDDSI website (www.iddsi.org).
IDDSI Food Classifications Are A Robust Development
Per their standards, a transitional food is defined as a “food that starts as one texture (e.g. firm solid) and changes into another texture specifically when moisture (e.g. water or saliva) is applied, or when change in temperature occurs (e.g. Heating). The physiological rationale for this level of thickness is that “biting is not required; minimal chewing is required and the tongue can be used for development teaching or rehabilitation of chewing skills (e.g. development of chewing in the pediatric population and/or developmental disability; rehabilitation of chewing function post stroke). Food specific examples include wafers, some biscuits/cookies/crackers etc.” (Source: IDDSI.org)
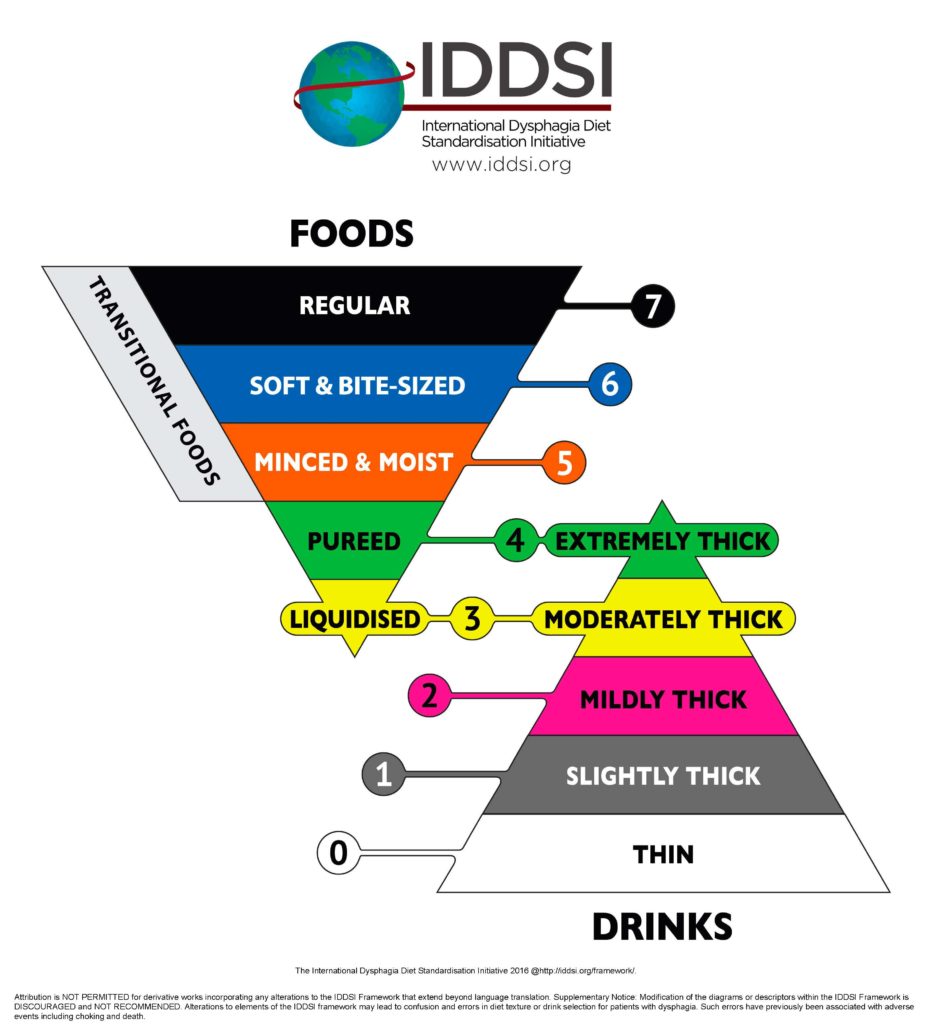
Scientifically standardizing food is seen as a positive development for many speech language pathologists. It provides a framework for people with dysphagia, their caregivers, clinicians, and the food service industry language to describe texture modified foods in a systematic way. The IDDSI framework indicates that a clinician may suggest a transitional food to be used with a level 7 (regular) diet to a level 5 (minced- moist) diet. Clinicians may also decide to introduce transitional foods in therapy as a tool for someone who is currently on a pureed diet and working to advance toward solids.
The EAT Bar Is Put To The Test
This summer, Nutraphagia’s EAT Bar was honored to be mentioned on Swallowstudy.com in an article by Karen Sheffler MS CCC-SLP, BCS-S, an expert in our field and board-certified specialist in swallowing and swallowing disorders.
In the selected excerpts below from her article “Cotton Candy Therapy? Transitional Foods & Dysphagia” (reprinted here with permission), Sheffler uses the EAT Bar as a product example for testing methods of transitional foods and as a possible therapy tool for discontinuing a pureed diet.
Testing Transitional Foods
Play with your food! In order to analyze the safety of transitional foods for your patients and loved ones, you have to play with it, in other words – test it. In addition to this testing method below, you need to put it in your mouth and feel it. Can you hold it in your mouth with minimal tongue pumping and it just dissolves?
1) Apply 1 ml of water to the sample. (Done here via syringe.)

2) Wait 1 minute.
3) Perform the IDDSI Fork Pressure Test (or chopstick test or finger test as described by IDDSI):

a. Use a standard fork
b. Apply pressure to the base of the fork with your thumbnail until your thumbnail blanches white (as in the picture below).
c. The sample should melt, disintegrate or squash and leave indentations from the fork. It does not return to its original shape when the pressure is released.
Now that you understand how the food feels in the mouth and throat, what oral processing skills may be needed, and how much moisture, heat and pressure is needed to break it down — you are ready to think about using different transitional food items in therapy.
Transitional Foods in Dysphagia Treatment
One pillar of dysphagia treatment is diet modification; however, this cannot be done without the other pillars of compensatory strategies and rehabilitation/skill training. How do we train skills to upgrade a person’s diet without causing a choking episode on that “training” piece of chicken?!
Can transitional foods be used to more safely train these biting, chewing, lingual lateralization and bolus formation skills needed for more challenging foods? Can they also be used to advance a diet in cases of oral sensitivity and solid food refusals (often seen in the pediatric and geriatric populations)?
A Transitional Food – Product Example:
(Disclosure again: I am not receiving any financial incentive to mention this product.)
This transitional food blog was inspired by me tasting, testing and analyzing a product called EAT Bar, by Nutraphagia. Co-founder, Tia Bagan, MS, CCC-SLP, sent me some products to sample; and, me and my family were hooked. My son ended up eating so many of them, that when I pulled out the chocolate package to have my 93-year-old mother-in-law try them, there was less than 1/2 of a biscuit left. My son and I are partial to chocolate anything, but the other flavors were delicious too. These are definitely a treat, and not for people with diabetes. The product is made in a facility that contains wheat, milk, eggs, coconut and soy. The product itself contains milk; but, has a “kosher supervision of America” seal on it. It is a product of Canada.
These yummy snacks have the potential for improving quality of life for people working to get off of pureed foods. They also may increase the acceptance of an easy to swallow solid for children through geriatrics with refusals, oral sensitivities or intake disorders (e.g., ARFID/Avoidant/Restrictive Food Intake Disorder). Swallowing evaluation and treatments should always be done under the guidance of your medical team that includes your speech-language pathologist who specializes in dysphagia. That is a matter of life or death! (That said, more on hazards and choking risks in Part 2 of this blog).
This product passed the IDDSI Fork Pressure Test when 1ml of water was added (see pictures and methods above). When I tested a bite, I tried to just hold it in my mouth and use as little oral preparatory movements as possible. I did not chew at all. I found that I needed only a little tongue pumping or up and down movements. The bite started to change shape and consistency within 10-12 seconds. Then it dissolved into a smooth paste by 22-25 seconds. By 30 seconds, I just needed to use my tongue to clear trace residue off my palate. After a few swallows, the bite cleared within 35 seconds. (Note: I tested this several times with fresh biscuits and with biscuits that had sat opened for weeks. Timings will vary with the individual.)
My son was good at testing too (and for reference, he is 11 years old). He hardly moved his jaw or tongue while holding the bite in his mouth. He showed me how the bite was starting to melt and deform at 27 seconds. Then at 38 seconds he showed how there was some residue on his palate. And yes, he said the word “palate.” After a few swallows, he showed how it was gone at 45 seconds. He was observed to do 5 swallows total, with the first swallows of saliva during the holding period. Right before he took another bite, he said: “It’s gone. Totally gone. Yeah, this is good!”
My first reaction was that it took some sucking and tongue pumping movements, but certainly easy to swallow, as you do not have to chew or lateralize the tongue. Because the biscuit is easy without chewing or using tongue lateralization, it could be used in therapy to safely train these skills.
NOTE: Please go to Cotton Candy Therapy: Transitional Foods as Potential Dysphagia Treatments for the complete article by Karen Sheffler MS CCC-SLP, BCS-S.
The Future Is Delicious
Additional and on-going research is needed to assess transitional foods and their use with our patients. It is an exciting time of innovation in the field of speech pathology. Nutraphagia is committed to playing a role and providing ongoing support for transitional food innovations.
We invite you to become part of our mission to bring joy, delight and care to everyone’s every day. Learn more about the EAT Bar at TheEATBar.com or @TheEATBar on Facebook and Instagram.
References
Sharon (Feb 5, 2013). Transitional Foods.
Retrieved from http://www.homegrown&healthy.com
Schwartz, Marnie (Sept 26, 2016). How “Certified Transitional” Foods Change the way you buy Organic Foods. Retrieved from http://www.shape.com
Sheffler, Karen (Aug 16, 2018). Cotton Candy Therapy? TransitionalFoods as Potential Dysphagia Treatments. Retrieved from http://www.swallowstudy.com
International Dysphagia Diet Standardization Initiative. Retrieved from http://www.iddsi.org





