Interpreting Labels
Have you ever experienced a situation where you try on two items of clothing or two pairs of shoes, both labelled as being the same size, only to discover that they actually fit differently?
How about ordering two cups of “dark” coffee sourced from different countries, only to experience that they have very different tastes?
Or how about trying to purchase matching paint when you don’t have the color code for the paint already on your wall? Two paints labelled with the same color name can be quite different…
These every day examples speak to the fact that we use labels to identify items that share similar characteristics, but differences can still exist within those labelled categories. Some of those differences may be barely noticeable while others stand out as obvious.
This general state of affairs is true for clothing sizes, taste characteristics, and colors. It is also true for the categories of liquid consistency and food texture that a clinician might recommend for a person with dysphagia. And, it can also be true across different production runs of a single commercial food product, such as a thickened beverage for people with dysphagia.
Early Approaches to Liquid Modifications
The practice of modifying food and liquid consistencies as a means of facilitating safer and/or more efficient swallowing has been around since the beginning of the field of dysphagia (1, 2). With liquids, the general principle is that thicker liquids flow more slowly than thin liquids, allowing the patient additional time with which to achieve airway protection. But clinicians and patients need more guidance: How thick is thick enough? Is there such a thing as too thick? When liquids differ in thickness, should we be worried? and How big does a difference need to be to be clinically meaningful? (3, 4)
Early approaches to categorizing liquid thickness referred to the clinically-relevant property as “viscosity”. The National Dysphagia Diet [NDD] (5) proposed four degrees of liquid consistency, with viscosity ranges (in centipoise or milliPascal seconds) of 0-50 (“thin”), 51-350 (“nectar-like”), 351-1750 (“honey-like”) and > 1750 (“spoon-thick” or “pudding”). When the NDD was adopted in North America, manufacturers of commercially available thickeners or pre-thickened products adopted the NDD text labels. Consumers of those products, including clinicians and patients, interpreted these labels to mean that products fell within the labelled categories. However, detailed information regarding the viscosity of a particular product, or exactly where it was expected to fall within the range of a particular category were rarely reported. As a result, two products with a small difference of 5-10 mPa.s might be labelled as falling in different categories, if their viscosities fell on either side of a category boundary, whereas two products with a much larger difference might be labelled as the same, depending on where their actual viscosity fell along the continuum.
However, measuring viscosity properly is far from simple. The task requires expensive instruments (rheometers) and precise methods to load tiny samples of liquid onto the testing plate, making sure there are no lumps or bubbles.

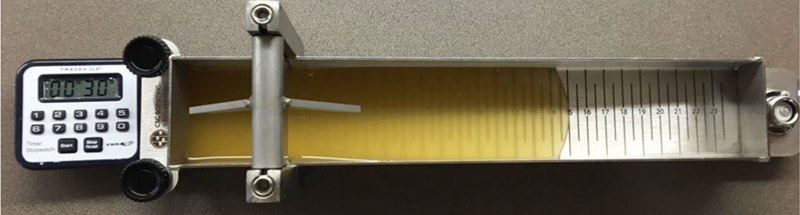
Temperature must be controlled, and for liquids with “non-Newtonian” properties, the measurements must be made across a wide range of shear rates (note that the viscosities proposed in the NDD were quoted at a single shear rate of 50 reciprocal seconds). Given that neither rheometers nor the expertise required to operate them are accessible in hospital kitchens or clinics, the users of commercially available thickened liquids for people with dysphagia were left with little choice other than to take the labels at face value. Another approach, adopted in some facilities and even by some regulatory bodies, was to seek simpler methods of measuring liquid thickness, such as Bostwick consistometers or line-spread devices (6-9).
The Devil Lies in the Details
Regardless of the measuring device, the truth about liquid thickness is that the proverbial devil lies in the details. Viscosity is not a linear phenomenon, so the relative magnitude of a 5 or 10 mPa.s difference is not the same at lower versus higher ends of the continuum. Furthermore, the viscosity of a liquid will differ depending on temperature, and for starch-thickened liquids the viscosity will change with time, or when the product becomes mixed with salivary amylase. How fast a liquid with a given viscosity actually flows depends on the forces that are applied to that liquid. This means that the same liquid might behave differently in two different patients, based on factors like the amount of tongue pressure applied during oral bolus transport.
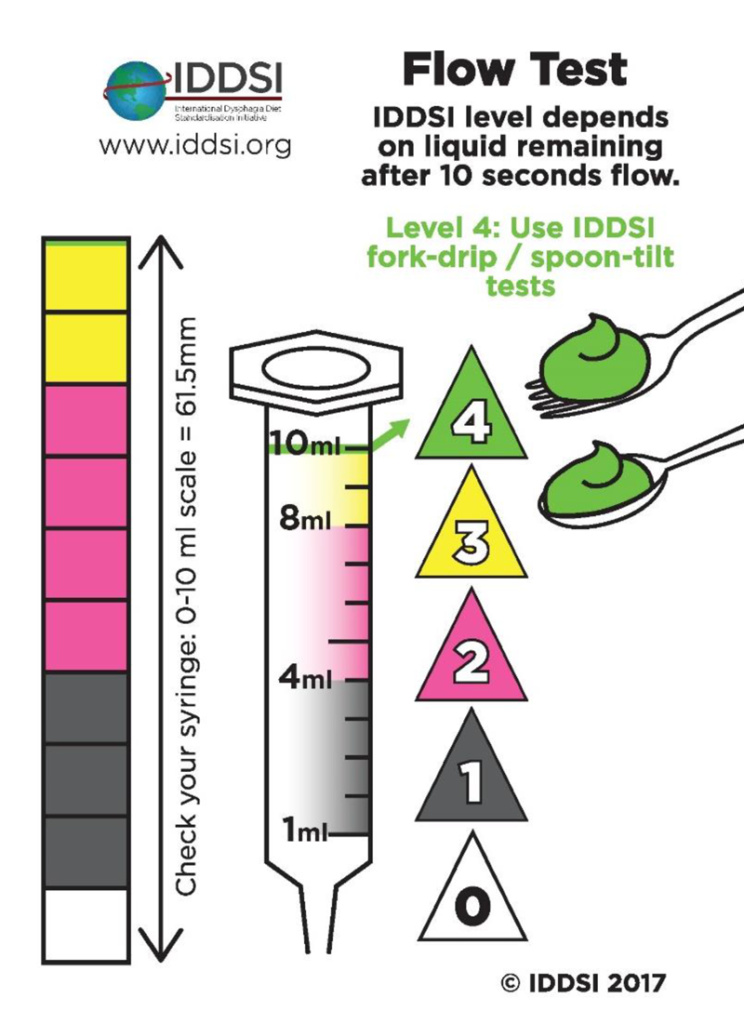
Different approaches to measuring liquid flow provide results in different units of measurement. Two liquids that appear to behave similarly using devices that measure flow across a level surface (e.g. a Bostwick consistometer) or under gravity (e.g. the IDDSI flow test) might actually have dramatically different viscosities when measured using a rheometer. When two liquids appear similar using one measurement approach but different using a second measurement approach, this does not mean that one of the measurement approaches is wrong. It simply means that the measurement approaches capture thickness in different ways, with different yardsticks! This is similar to comparing a given distance in miles to the number of steps or the time required for an average person to walk that distance – all 3 measures tell us something about the distance, but they do so in different ways. Although two liquids prepared with different thickeners may behave similarly using visuo-perceptual methods of appraisal (such as watching them pour off a spoon or out of a cup), and may display similar flow properties when measured using consistometry, line-spread tests or the IDDSI Flow Test, they are likely to have quite different viscosities when tested using a rheometer.
These realities may make clinicians feel uncomfortable about their role in recommending liquid thickness for a patient with dysphagia. The recent introduction of the IDDSI Flow Test has empowered clinicians, caregivers and patients to appreciate very small differences in flow between liquids. A growing number of users are starting to ask about the relative importance of such differences.
Things to Remember When Recommending Liquids for People with Dysphagia
Here are some thoughts to take into consideration when recommending liquid thickness for a patient:
- It is impractical to target very specific points on the continuum (e.g., an IDDSI flow test result of 2.5 mL remaining in the syringe after 10 seconds of flow).
- It is much more practical to recommend a range of thickness that is suitable for a patient, enabling them to use a variety of products within that range.
- Ranges of liquid thickness have always been there – this is not a new reality.
- Temperature matters! Most liquids will become thicker as they cool.
- It is simply not possible for a clinician to exhaustively test small increments of liquid thickness in videofluoroscopic swallowing assessment. To do so would expose the patient to unacceptable amounts of radiation.
- Best practice in videofluoroscopy is to use standard stimuli that are representative of ranges of liquid thickness (such as the different levels of liquid thickness in the IDDSI framework).
- Remember that the same patient might swallow two boluses of the same liquid differently.
- Recommending a range of liquid thickness for a patient does not guarantee that the patient will necessarily do well with all liquids that fall inside that range. Further tailoring of recommendations may be needed for a given patient based on observation of their swallowing.
- Such explorations of a person’s swallowing across a particular range of thickness can be done during clinical or endoscopic swallowing assessments.
- Recommendations can also be tailored according to other relevant factors such as the patient’s level of alertness or fatigue at different times of day, or relative to their medication cycle.
- Research has yet to identify the size of a minimally-relevant difference in thickness or to find particular points along the thickness continuum that represent boundaries between risky or safe liquids for people with dysphagia (10). In fact, finding such boundaries seems unlikely given the diversity we see in people with dysphagia.
Best Practice Suggestions
So, what should a clinician do when trying to determine an appropriate recommendation for a person with dysphagia? Here are the recommended steps:
- Use standard assessment practices to confirm whether a patient experiences difficulty with thin liquids like water.
- If a patient displays difficulty with thin liquids, evaluate the impact of progressive increments of thickening.
- The IDDSI Framework provides ranges that can be evaluated in sequence, beginning with slightly thick liquids.
- In videofluoroscopic assessments, standard barium stimuli representative of each level should be tested according to a standard protocol.
- Reference values for expected swallowing physiology on videofluoroscopy exist for the 5 IDDSI levels of liquid thickness (11).
- For quality of life and to avoid risks of greater residue and dehydration, the goal should be to avoid over-thickening.
- Once appropriate thickness levels for a patient have been identified using standard stimuli, further exploration of other liquids from the same and adjacent levels can be performed through non-radiographic methods of assessment.
Final Thoughts
The thickness label of a particular item is just that – a descriptive label. It should never be interpreted to imply or guarantee effectiveness of that product for improving swallowing in a particular patient. The only thing a label tells you, is whether the product claims to fall (or not fall) in a range of thickness that has been identified by a clinician as being suitable for the patient. Even when there is a label on a product, clinicians should remain alert to the possibility that a product will vary with temperature and may vary from batch to batch or based on factors like shelf life. If a product does not seem to be performing as expected, the IDDSI testing methods provide the clinician or caregiver with a means to confirm the consistency of a product at the point of serving.
References
- Coster ST, Schwarz WH: Rheology and the swallow-safe bolus. Dysphagia 1: 113-118, 1987.
- Logemann JA: Evaluation and treatment of swallowing disorders., 2nd ed. San Diego, CA: College Hill Press, Inc., 1997.
- Cichero JA, Jackson O, Halley PJ, Murdoch BE: How thick is thick? Multicenter study of the rheological and material property characteristics of mealtime fluids and videofluoroscopy fluids.
Dysphagia 15: 188-200, 2000. - Cichero JA, Jackson O, Halley PJ, Murdoch BE: Which one of these is not like the others? An inter-hospital study of the viscosity of thickened fluids. J Speech Lang HearRes 43: 537-547, 2000.
- Force NDDT: National Dysphagia Diet: Standardization for Optimal Care/American Dietetic Association: Diana Faulhaber, 2002.
- Barbon CEA, Steele CM: Thickened Liquids for Dysphagia Management: a Current Review of the Measurement of Liquid Flow. Current Physical Medicine and Rehabilitation Reports, 2018.
- Cote C, Germain I, Dufresne T, Gagnon C: Comparison of two methods to categorize thickened liquids for dysphagia management in a clinical care setting context: The Bostwick consistometer and the IDDSI Flow Test. Are we talking about the same concept? J Texture Stud 50: 95-103, 2019.
- Garcia JM, Chambers Et, Matta Z, Clark M: Viscosity measurements of nectar- and honey-thick liquids: product, liquid, and time comparisons. Dysphagia 20: 325-335, 2005.
- Budke J, Garcia JM, Chambers EIV: Comparisons of Thickened Beverages Using Line Spread Measurements. Journal of the Academy of Nutrition and Dietetics 108: 1532-1535, 2008.
- Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, Coutts K, Dantas RO, Duivestein J, Giosa L, Hanson B, Lam P, Lecko C, Leigh C, Nagy A, Namasivayam AM, Nascimento WV, Odendaal I, Smith CH, Wang H: The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia 30: 2-26, 2015.
- Steele CM, Peladeau-Pigeon M, Barbon CAE, Guida BT, Namasivayam-MacDonald AM, Nascimento WV, Smaoui S, Tapson MS, Valenzano TJ, Waito AA, Wolkin TS: Reference Values for Healthy Swallowing Across the Range From Thin to Extremely Thick Liquids. Journal of Speech, Language, and Hearing Research 62: 1338-1363, 2019.





