Parkinson’s Disease and dysphagia: Timing matters

Introduction
Last year, after reporting some swallowing difficulties to her primary care physician, a friend of mine, Kate, was referred for a swallow study, which turned out to be a barium swallow study. Kate, an award-winning blogger, has lived with Parkinson’s disease for 18 years and for nearly half of that time, has benefitted from DBS (Deep Brain Stimulation) surgery.
Prior to the study, she was told that she must be NPO. It didn’t occur to her to ask if this included her medications. By the time the scheduled test occurred, she had been off her Parkinson’s medications for 12 hours and arrived for the procedure stiff and moving slowly. Because a barium swallow study was conducted, she was eventually required to drink thin barium prone and supine, at which point she aspirated. She was informed by the referring physician that she had “failed” the swallow study, and because of the witnessed aspiration, sent to an ENT. The ENT found nothing wrong, and advised she return if her swallow function declined. She was then referred for a modified barium swallow study, which was completed upright and on meds, and no aspiration was observed. Kate relayed the scenario to me afterward, and asked if there was anything she could be doing to improve her swallowing function.
Parkinson’s and dysphagia
Dysphagia can develop at any point during Parkinson’s disease, with reported frequency ranging from 30% to 82%. Objective tests, however, indicate a higher frequency of dysphagia, and this may be because patients may be asymptomatic and unaware of their swallowing difficulties until later in the disease course. Newer models of PD have identified Lewy bodies in non-dopaminergic brainstem and cortical areas (swallowing control areas), and therefore suggest that a subclinical dysphagia can be one of the early symptoms.1
It has also been reported that persons with PD may be more likely to swallow at abnormal times within the respiratory cycle, and more likely to inhale after swallowing, even when swallowing during the exhalation phase. This lack of proper coordination of breathing and swallowing has been proposed as an important underlying factor for dysphagia, placing patients with PD at increased risk for aspiration.2
What is the effect of Parkinson’s medications on swallowing?
Levodopa and dopamine agonists are the first lines of defense against PD, and are very capable of improving and controlling symptoms for several years. Various other dopamine agonist medications have been developed over the last few decades, with the goal of prolonging the beneficial effects of dopamine on motor symptoms. Over time, however, despite medications, it is estimated that 40% of persons with PD will experience motor fluctuations within 4-6 years of onset, increasing by 10 percent per year after that. Fluctuating dopamine levels also affect non –motor features such as fatigue, depression, and anxiety.3
The effects of Parkinson’s medications on dysphagia has been controversial or inconclusive, with several studies reporting that Apomorphine, a dopamine agonist which is injected subcutaneously, alleviated dysphagia in some patients with PD. More recently Rotigotine, another dopamine agonist with non-oral administration as a transdermal patch, has been reported to exert some beneficial effects on swallowing in some persons with PD. 4
When evaluating and/or treating patients with Parkinson’s disease, it is important for the SLP to ask about medications, “on/off” symptoms that the patient might be experiencing, and be sure that an instrumental swallow study, whether MBSS or FEES, is conducted with the patient in an “on” state for optimal performance.
DBS and swallowing
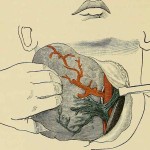
Deep Brain Stimulation (DBS) surgery is a surgical procedure consisting of the placement of an electrode into one of several possible targets in the brain, aided by computer guidance and 3-D physiological mapping. Typically DBS has been performed in people with Parkinson’s disease after medication trials are no longer effective for controlling motor symptoms many years into their disease. More recent studies, however, have suggested that DBS performed earlier in the disease process may yield improved motor control, improved quality of life, and comparable adverse side effects with resolution, as compared to medication treatment alone.5 The exact target for DBS, however, is somewhat controversial, and optimal placement of the electrodes, and post DBS programming, is important not only for management of motor symptoms, but also with regards to the effect of DBS on speech and swallowing.
The research looking at the effect/s of DBS on swallowing does not yield consistent findings. Some researchers have reported that bilateral STN-DBS does not substantially impair swallowing in PD 6, while others have reported that the idiosyncratic side effects such as dyskinesia or dystonias can occur post DBS and may impact the timing and coordination of breathing and swallowing.7
A systematic review of DBS effect on swallowing was conducted and reported by Michelle Troche et al, University of Florida.8 This literature search identified 13 studies specifically addressing the effects of DBS on swallowing and concluded that there was a lack of consensus regarding improvement or decline in swallow function post DBS, suggesting that this was likely due to different research design and methods. Consequently, in their conclusions, it was suggested that consistent methods be employed when researching this issue including: lead locations (i.e. STN v/s GPi), bilateral v/s unilateral DBS, programming stability, on/off medication considerations, and proper evaluation techniques.
These same considerations are important for the SLP when evaluating and treating dysphagia in patients with DBS as well. Additionally, because patients may not always be aware of dysphagia, it is important that an instrumental swallowing study be conducted prior to DBS surgery, so that a baseline for change has been established.
Treatment approaches
Given reports in the literature, I will assume that many persons with PD are not even evaluated for dysphagia until they become symptomatic, or, worse case scenario, develop aspiration pneumonia. Like my friend Kate, some may have no evidence of aspiration on an MBS study, and so are sent on their way with no recommendations for preventative exercise/s, such as expiratory muscle strength training, and/or instruction in breathing technique which may help improve timing of breathing and swallowing.
Speech-language pathologists/dysphagia therapists are increasingly addressing swallowing problems with preventative models of treatment, and similar to our Physical Therapy (PT) colleagues, view this as a pre-emptive approach. Tai chi, yoga, dance, are a few of the classes a physical therapist or neurologist might recommend to a person with PD as a means of reducing fall risk, maintaining mobility, etc.
Similarly, instead of waiting for persons with PD to be referred for dysphagia evaluation and intervention, I propose that speech-language pathologists adopt a similar approach to PT, and incorporate breathing and swallowing exercises into group classes and other community-based programs for persons living with PD. Having employed this approach for several years now, I have found it to be an excellent way to provide ongoing education, instruction in exercises and compensatory strategies that might facilitate safer and more efficient swallowing function. This type of community-based programming often increases awareness, leading individuals to self-identify as having a swallowing problem that they might not have otherwise discussed with their neurologist or primary care physician.
Despite all of the treatment advances in Parkinson’s, aspiration pneumonia remains a major cause of death in PD. The role of the SLP in continuing to bring awareness about swallowing issues and treatment strategies in this population cannot be underestimated
References
- Miller N, Noble E, Jones D, Burn D. Hard to swallow: dysphagia in Parkinson’s disease. Age Ageing. 2006;35:614–618.
- Gross RD, Atwood CW, Jr, Ross SB, Eichhorn KA, Olszewski JW, Doyle PJ. The coordination of breathing and swallowing in Parkinson’s disease. Dysphagia. 2008;23:136–45
- Source: Parkinson’s Disease Foundation www.pdf.org/
- Hirano, et al. Rotigitine Transdermal Patch Improves Swallowing in Dysphagic Patients with Parkinson’s disease. Dysphagia 2015 30:452-456.
- Source: DBS 4 PD.org http://www.dbs4pd.org/researchphp
- Silbergleit, Alice K., et al. “Comparison of dysphagia before and after deep brain stimulation in Parkinson’s disease.” Movement Disorders 27.14 (2012): 1763-1768.
- Oluwakemi Y. Fagbami,M.D., and Anthony A. Donato, M.D., Stridor and dysphagia associated with subthalamic nucleus stimulation in Parkinson disease. Journal of Neurosurgery Nov 2011 / Vol. 115 / No. 5, Pages 1005-1006
- Troche, Michelle S. et al. Swallowing and deep brain stimulation in Parkinson’s disease: A systematic review. Parkinsonism & Related Disorders , Volume 19 , Issue 9 , 783 – 788