A newer clinician in a SNF is nervous about what PDPM means for the way she currently treats her patients. Her DOR and the webinars she’s been watching have focused on the use of evidence-based interventions to provide the best outcomes for her patients without wasting therapy minutes on those interventions that have been shown not to work. She’s already scheduled very tightly in her day and is overwhelmed by the prospect of yet another task, let alone a daunting one like evidence-based practice (EBP).
This clinician is not alone. As October 1 approaches, PDPM (patient driven payment model) is looming large in the mind of many clinicians. PDPM is a fundamental shift in the way that skilled nursing facilities are reimbursed through Medicare. Under the current system, SNF reimbursement is tied to therapy utilization resulting in higher payments for more minutes of therapy. The new PDPM system shifts the focus back to the patient and provides an opportunity for greater collaboration between rehab and nursing team members. Payment is based on a patient’s clinical characteristics and anticipated needs rather than how many minutes of which type of therapy they receive (CMS, 2019). With this new model’s emphasis on quality over quantity of care, using evidence-based treatment approaches will become even more essential.
The mean productivity requirement for skilled nursing facilities is 85% (ASHA, 2017). This means there isn’t enough time in the day to treat your patients, document, collaborate with other professionals and use the bathroom let alone spend hours upon hours combing through individual studies seeking out the most up-to-date research on dysphagia.
The clinician in the above scenario needs high-quality information and she needs it fast. ASHA understands the time-crunch and has developed Evidence Maps to do the legwork for you. This dedicated member resource appraises, summarizes, and categorizes relevant literature to save you your most precious resource: time.
The Evidence Maps contain the most up-to-date research that addresses clinical topics in speech-language pathology and audiology. The Maps organize systematic reviews, meta-analyses, clinical practice guidelines, and ASHA practice policies according to clinical topic to make the articles easy to find. Below, you’ll see the Evidence Maps home page which contains many clinical topics including both pediatric and adult dysphagia. Let’s walk through an example of how this clinician can use the maps to ensure her treatments are evidence-based.
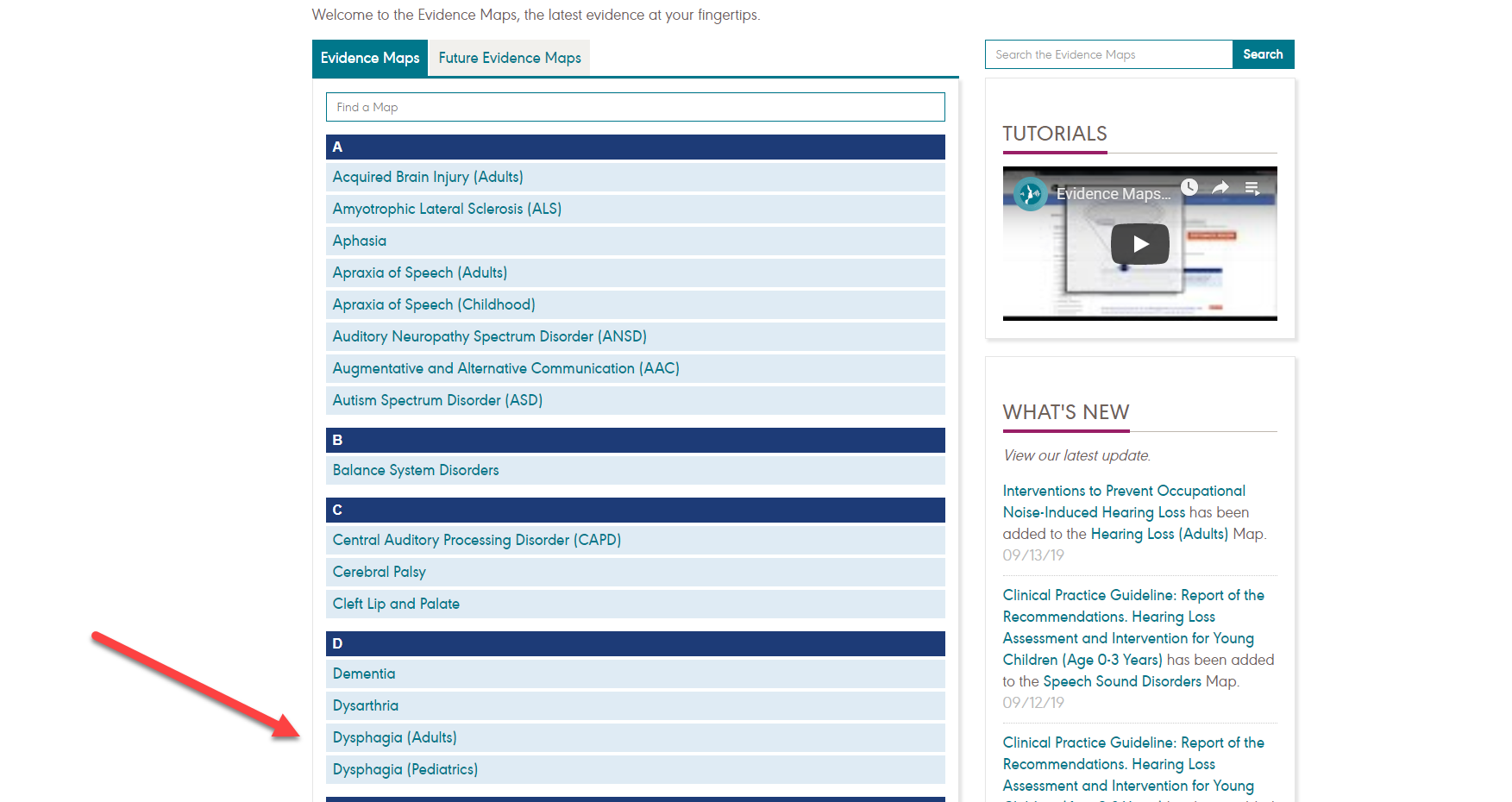
Because our clinician is working in a SNF we selected the adult dysphagia map. As you can see below, our search initially returns 196 articles divided into three tabs (yellow arrows) for the three components of EBP: external scientific evidence (research), clinical expertise (guideline recommendations based on expert consensus) and finally client perspective.
So many articles can be a bit daunting. She can narrow down her findings by using the filters on the left (red arrows) to find articles pertaining to her specific practice area (assessment, screening, treatment or service delivery) and population (based on diagnosis). The green arrows below show where she can find a brief description of the article as well as its conclusions relevant to SLPs.

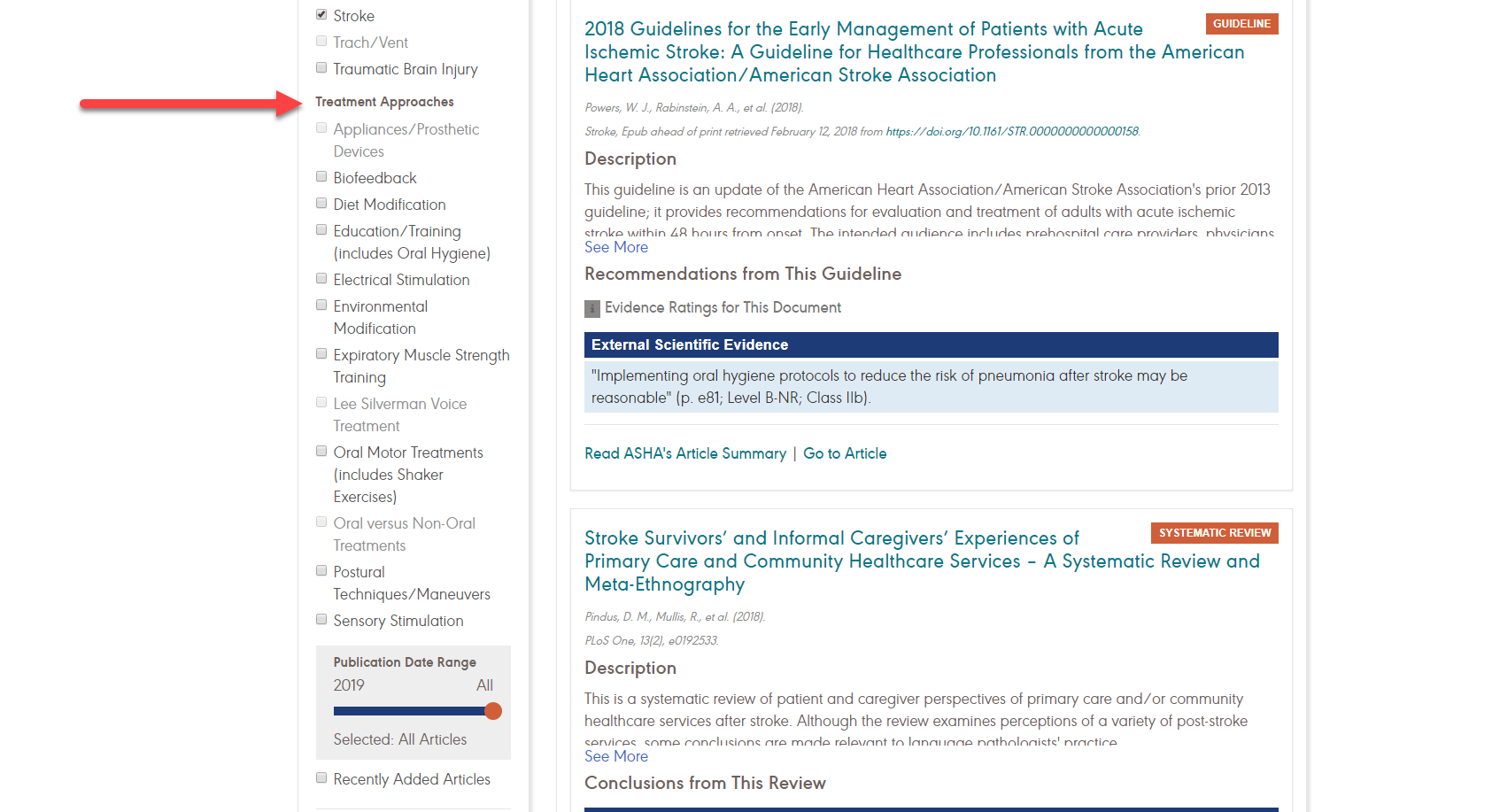
Let’s say our clinician is interested specifically in swallowing treatment interventions for her patients recovering from a stroke so she selects the treatment and stroke boxes. Applying these filters narrows down her findings to a much more manageable 34 articles. From there she won’t have to read all 34 research articles but can merely scan the descriptions and conclusions to determine which ones are most applicable to her patient.
The Evidence Maps can also be used to examine the wide variety of treatment approaches for adults with dysphagia including expiratory muscle strength training, diet modifications, postural techniques/maneuvers and electrical stimulation. She can click on each individual treatment to see the available external scientific evidence, clinical expertise and client perspectives to determine if the approach in question is evidence based and has been shown to work for individuals with similar characteristics to her patient.
Using this resource, the entire process takes a few minutes instead of hours upon hours of searching, sifting, appraising and extracting relevant conclusions. ASHA have already done this work so you don’t have to.
While each patient requires individualized goal planning and consideration, the Evidence Maps offer you a guide to get from evaluation to outcomes with solid research to help you determine which interventions you can trust.
Helping patients achieve their desired outcomes without wasting their time is essential as health care payments move away from billable minutes and toward value-based care. PDPM as well as PDGM (the new home-health payment model taking effect January 1, 2020) strive for maximum benefit for the dollars spent (Warren, 2018). SLPs need to be able to defend their treatment as skilled, necessary and beneficial, there is no time to waste on interventions that don’t show improvement. Evidence-based practice gives you solid ground to stand on if payers or administrators question your treatment decisions. It also empowers you to provide your patients with the highest quality care to reach their swallowing goals.
References
ASHA (2017). 2017 SLP health care survey summary report: Number and type of responses. Retrieved September 19, 2019, from https://www.asha.org/uploadedFiles/2017-SLP-Health-Care-Survey-Summary.pdf
Centers for Medicare & Medicaid Services (2019). Fact Sheet: PDPM Patient Classification Baltimore, MD. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/PDPM.html#resources
Warren, Sarah (2018). Medicare Proposes Overhaul to Home Health Payment. The ASHA Leader, 23(9), 24-25.





