This content is sponsored by Passy-Muir
Following medical diagnosis and intervention, complications may arise for a patient which trigger referrals to a speech-language pathologist (SLP). These consultations often call on the SLP’s expertise in evaluating and treating speech, language, swallowing, communication, and cognition, among others. However, these broader areas of focus also require that the SLP assess the more nuanced areas impacted, investigating contributing factors that may affect the plan of care, such as airway patency.
What is airway patency?
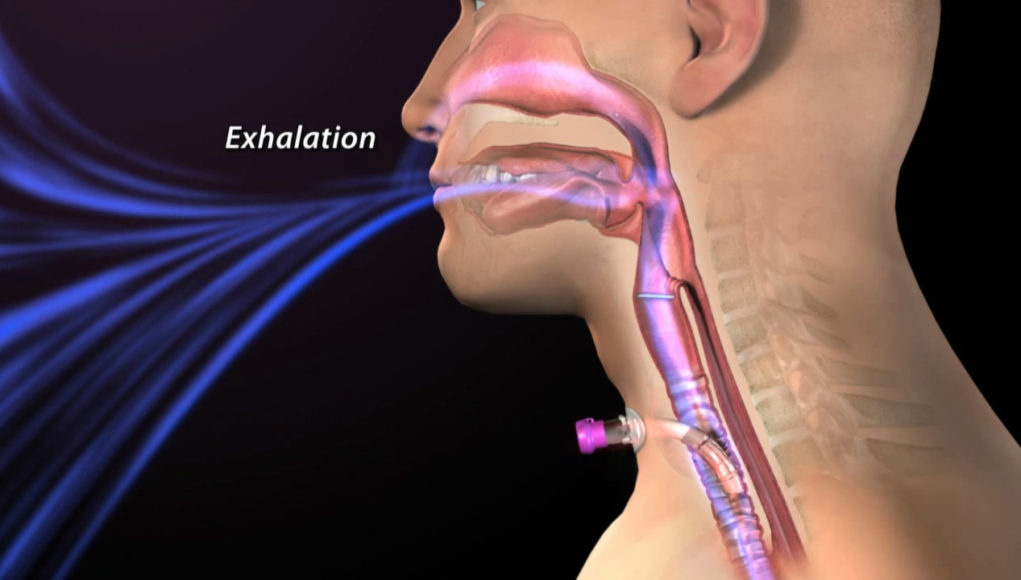
Simply put, airway patency is the ability of a person to breathe, with airflow passing to and from the respiratory system through the oral and nasal passages. Airway patency may be impacted by anatomical or physiologic changes that impede airflow or even by a foreign object, such as a tracheostomy tube. These factors become particularly relevant to speech language pathologists when the mechanisms for maintaining airway patency are affecting the ability to swallow. The relationships between upper airway function, intra-oral and intra-pharyngeal pressure, and activation of the muscles involved in respiration all interact during swallowing. Because of this direct relationship with swallowing, understanding airway patency is critical.
Airway patency is assessed by evaluating for the presence or absence of obstructive signs or symptoms that suggest the airway either is or may become obstructed. Signs and symptoms include such findings as stridor with breathing, secretions, snoring, difficulty with inhalation and/or exhalation, coughing, and changes in respiratory status, such as decreased oxygen saturations. Obstruction may occur due to injury with edema, direct trauma to the airway, neurologic impairment, inhalation or swallowing of a foreign object, allergic reaction, tumors, vocal fold changes, viral or bacterial infections, abscesses to the tongue or epiglottis, bronchitis or pneumonia, COPD, smoke inhalation, and many others. Some of these causes may lead to emergent or planned intervention, such as intubation or tracheostomy, to provide more direct access to breathing and to bypass the obstruction.
When is airway patency a consideration with tracheostomy?
The changes that occur to communication and swallowing following tracheostomy have been well-documented (Barrow and King, 2020; Freeman-Sanderson, Togher, Elkins and Kenny, 2018). Airway patency is an immediate consideration following tracheostomy as it has the potential to negatively impact various functions, such as cough, throat clear, voice, and swallowing.
Typically, when a tracheotomy is first performed, the general standard is to place a Shiley, cuffed tracheostomy tube in a size 8. In Figure 1, a size comparison of the human trachea to the most common tracheostomy tube brands is provided. Of note is that the outer diameter (OD) and inner diameter (ID) of each tracheostomy tube varies when compared to other brands. While it is common to use a size 8 tracheostomy tube with initial placement without regard to gender, a distinct difference in the size of the trachea exists between genders, with the female trachea being much smaller than a male trachea, average range for females being 12.5 mm to 15.7 mm and for males 15.6 mm to 19.6 mm (Khade, Yadav, and Divan, 2016).
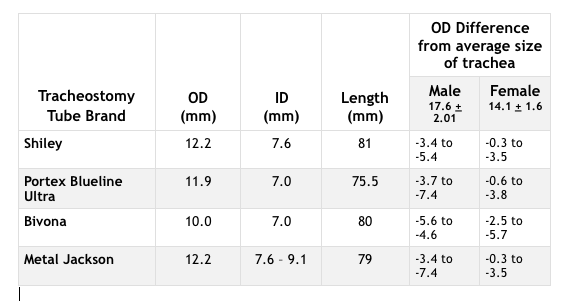
When considering airway patency, the ability to pass air through the trachea is paramount. With the outer diameter of a tracheostomy tube causing a partial occlusion in most and potentially complete occlusion of the airway in others, knowing the state of patency becomes a critical piece of information.
As an SLP initiates a swallowing evaluation with a patient following tracheostomy tube placement, one of the first steps of that evaluation is to assess airway patency. Knowing the status of a patient’s airway patency will provide information relevant to options, for both swallowing assessment and interventions. From a swallowing standpoint, how might the ability to throat clear and cough potentially assist with protecting the airway during swallowing? Is a speaking valve an option that will assist with restoring subglottic pressure, sensation, hyolaryngeal excursion and other functions impacting swallowing (for a more detailed review, see the article by Barrow, 2020)?
How to assess airway patency?
When a patient has a tracheostomy tube, several options exist for evaluating airway patency. The method used is dependent on whether a patient is on mechanical ventilation or is a spontaneous breather and not on a ventilator. When a patient is on mechanical ventilation, Sudderth (2016) shared:
“Once the cuff is completely deflated, airway patency can be determined by assessing voicing on exhalation, listening for exhalation though the upper airway using a stethoscope, or by reading the peak inspiratory pressure (PIP) and/or exhaled volumes via the ventilator. The clinician can objectively document an adequate leak and upper airway patency when reading a 40-50 percent drop in PIP and/or decrease in exhaled tidal volume measured by the ventilator. These measurements would suggest that the tracheostomy tube is properly sized to allow for sufficient airflow around the tracheostomy and upwards to the upper airway. It also suggests that there is no significant obstruction above the tracheostomy tube. A no-leak speaking valve then can be placed into the ventilator circuit while mechanical ventilation continues.”
If the patient is not on mechanical ventilation, then two of the options include listening for voicing with cuff deflation (or with cuffless tracheostomy tube) or using finger occlusion. Finger occlusion involves the clinician deflating the tracheostomy tube cuff, if present, then occluding the tracheostomy tube hub with a gloved fingertip. The clinician watches the patient’s respiration and occludes just after inhalation. Monitoring and observing exhalation to occur out through the mouth and nose indicates potential airway patency. If the patient achieves any voicing, a cough, or blows air out the mouth and nose, this indicates that the patient exhales air around the tracheostomy tube. If there is no voice or airflow, then the patient may have some or complete occlusion.
Another option is to use transtracheal pressure measurements (TTP) (for full review and description see Brooks, 2018). TTP is an objective method for measuring airway patency with tracheostomy tubes. It is a process involving the use of a manometer to measure the pressure that is occurring within the airway. Research has shown that when the TTP measurement is at 6 – 10 cmH2O, then the airway is patent and airflow past the tracheostomy tube occurs (Barraza, Fernandez, Halaby, Ambrosio, Simpser, and Pirzada, 2014; Utrarachkij, Pongsasnongkul, Preutthipan, and Chantarojanasri, 2005). TTP may be conducted during finger occlusion or with the use of a speaking valve, both on and off mechanical ventilation.
If an airway is not patent, then back pressure (also, called air trapping) may be observed. This occurs because what the patient inhales is not able to be exhaled sufficiently past the tracheostomy tube, causing pressure to build below the tracheostomy tube. The sign of back pressure that is observed occurs when there is a woosh of air released at the site of the tracheostomy hub when the finger is removed. Back pressure not only indicates that the airway is not patent but also may provide more clinically relevant or even diagnostically important information as to what is happening with a patient. Back pressure is a negative sign indicating occlusion. This occlusion may be anatomical, physiological, or due to placement of a tracheostomy tube in situ. Determining the cause provides pertinent information affecting the next steps in the care plan.
It is when an airway is not patent that further diagnostic steps must be taken by the SLP, as SLPs have a role in determining why back pressure happens. The first step for troubleshooting the issue is to look at the tracheostomy tube size. As seen in Figure 1, the tracheostomy tube may be as large or even larger than the trachea. If a patient has a minimal space due to the size, this puts the patient at more risk for mucosal tissue injury in the trachea, with the potential for problems such as stenosis, granulation tissue, and tracheoesophageal fistulas, especially if the cuff is not properly managed (King and Harrell, 2019). If the patient has a tracheostomy tube with a cuff, just the presence of the cuff may occlude the airway. The purpose of a cuff is to seal the airway for mechanical ventilation; therefore, if a patient is not on ventilation, then the cuff is most often not needed (King and Harrell, 2019).
If the issue is not caused by the tracheostomy tube, then additional investigation into anatomical changes, such as swelling or vocal fold injury; physiological impacts, such as increased work of breathing and secretions; and behavioral considerations, such as anxiety and stress, must be considered. Evaluating each area systematically allows the SLP to provide information to the team relevant to what the next steps may need to be for addressing the airway patency and improving the ability of the patient to exhale through the mouth and nose. Having a team approach provides a more comprehensive review of the patient’s systems. Respiratory therapy (RT) may address secretion issues, tracheostomy tube issues, or other respiratory factors that may impact airway patency. If the potential cause is not readily identified, then referral to a laryngologist (ENT) may lead to an endoscopic evaluation to assess for vocal fold function, edema, or other structural abnormality or change to better assess the cause. Determining the cause allows the appropriate intervention and contributes to the SLP assessment and intervention plan for swallowing, including the potential for using a speaking valve.
Why evaluate airway patency?
The functional significance of the respiratory-swallow coordination and interaction during the act of swallowing is far from fully understood. To swallow involves a synergistic relationship between multiple complex functions that involve the ability to generate pressure, subglottic, intra-oral, pharyngeal, and esophageal, and to assist with propelling a bolus through the aerodigestive tract while simultaneously protecting the airway (Martin-Harris, 2008). The airway is protected by movement of structures, subglottic pressure, respiratory control, and use of a cough and throat clear. This interdependent relationship between swallowing and respiration may already be compromised following a medical event, such as stroke, brain injury, head and neck cancer, and other diagnoses which may lead to airway patency issues. The complication of a tracheostomy just compounds the issue and further impacts the relationship of respiration and swallowing.
Not only is this relationship key during the act of swallowing, but the provision of behavioral modifications and compensatory strategies often involves the ability to modify respiratory behavior, including alterations in the respiratory-swallow coordination. Airway patency is the first step in addressing both the relationship of respiration to swallowing and the ability to intervene by manipulating the respiratory system. Alterations in respiratory-swallowing patterns have been shown to be associated with increased aspiration and swallowing difficulty (Martin-Harris, 2008). For this coordination to be optimal, the airway must be patent. For this reason, evaluating airway patency is a critical first step when initiating assessment of swallowing with a patient.
References
Barraza, G. Y., Fernandez, C., Halaby, C., Ambrosio, S., Simpser, E. F., & Pirzada, M. B. (2014). The safety of tracheostomy speaking valve use during sleep in children: A pilot study. American Journal of Otolaryngology, 35(5), 636-640.
Bartow, C. & King, K. (2020). Impact of a tracheostomy on swallowing. Dysphagia Café. Retrieved from https://dysphagiacafe.com/2020/09/24/impact-of-a-tracheostomy-on-swallowing/
Brooks, L. (2018). Infants and children with tracheostomy and ventilator dependence in the intensive care units: Candidacy and early intervention with a bias-closed, no-leak speaking valve. Aerodigestive Health. Retrieved from https://www.passy-muir.com/journal-3-1-dependence/
Freeman-Sanderson, A. L., Togher, L., Elkins, M. R., & Kenny, B. (2018). Quality of life improves for tracheostomy patients with return of voice: A mixed methods evaluation of the patient experience across the care continuum. Intensive Critical Care Nursing, 46,10-16. doi:10.1016/j.iccn.2018.02.004
Khade, B., Yadav, N., & Divan, C. (2016). Morphometry of the human trachea in male and female using a computerized tomography – a comparative study. Indian Journal of Clinical Anatomy and Physiology, 3, 526 – 530. Doi: 10.5958/2394-2126.2016.00121.3
King, K. & Harrell, M. (2019). Tracheostomy tube cuff considerations: Impact, management, and purpose. Dysphagia Café. Retrieved from https://dysphagiacafe.com/2019/10/14/tracheostomy-tube-cuff-considerations-impact-management-and-purpose/
Martin-Harris, B. (2008). Clinical implications of respiratory-swallowing interactions. Current Opinions in Orolaryngology, Head, and Neck Surgery, 16(3), 194 -199. Doi: 10.1097/MOO.0b013e3282febd4b
Sudderth, G. (2016). Speaking valve use during mechanical ventilation: More than just for communication and swallowing. Talk Muir. Retrieved from https://www.passy-muir.com/talkmuir-6-1-mechanical-vent/ .
Utrarachkij, J., Pongsasnongkul, J., Preutthipan, A., & Chantarojanasri, T. (2005). Measurement of end-expiratory pressure as an indicator of airway patency above tracheostomy in children. Journal of the Medical Association of Thailand, 88(7), 928-33.