This content is sponsored by Passy-Muir
Ideal scenario:
Let’s start with the ideal scenario the speech-language pathologist (SLP) hopes to encounter when receiving a consult for an evaluation for speaking valve use for communication and swallowing.
“Mr. Jones” is awake, alert, and medically stable. He has a size 6 cuffed Shiley tracheostomy tube. His nurse reports good secretion management and readiness for a Passy-Muir Valve assessment. As you enter the room, he is sitting up in bed, smiling and calm. His work of breathing, color, respiratory rate, heart rate, and oxygen saturations are stable. He listens attentively as education about the speaking valve (Passy-Muir Valve (PMV)) is provided. Since his medical status is stable, you proceed with your evaluation. Initiating slow cuff deflation and continued monitoring of baseline parameters, an airway patency assessment is completed. You determine that Mr. Jones exhales around his tracheostomy tube and out through his upper airway. With a patent airway, you place the PMV and continue your assessment. He demonstrates a productive cough to clear secretions. His vital signs remain stable. He begins speaking with a strong and clear voice. Precious words are exchanged between the patient and his family. He expresses his appreciation to you – speech-language pathologist extraordinaire – for giving him his voice back. Success!
Although, this type of wonderful, rewarding, immediate success is attainable with some patients, SLPs often encounter challenges which require more time, critical thinking, troubleshooting, and problem solving. Below are some of the more common problems clinicians face when assessing and treating patients with tracheostomy tubes, along with potential solutions to rectify the issue and reach the desired goal of successful PMV use.
Problem one:
The patient is unable to exhale through the upper airway, or in other words, the patient does not have a patent airway.
| Possible causes | Possible solutions |
| Fully inflated or partially inflated cuff. | Check that the cuff is completely deflated. Fully deflate the cuff by attaching a syringe and pulling back on the plunger until you meet resistance. |
| Tracheostomy tube size. | Review the size of the patient’s tracheostomy tube (found on the neck flange). Consider if downsizing the tracheostomy tube is an option. |
| Presence of a cuff. | Even if fully deflated, the cuff takes up space in the airway. Consider a cuffless tracheostomy tube, if medically appropriate. |
| Foam filled cuff | Foam filled cuff is an absolute contraindication for Valve use. Do not place a speaking Valve. |
| Upper airway obstruction. | Consider patient history and possibility for edema; thick, copious secretions; vocal fold injury or paralysis in the adducted position; upper airway tumor; tracheal stenosis; or tracheomalacia, among others. Consider referral to ENT for assessment. |
Problem two:
The patient coughs excessively with cuff deflation or Valve placement.
| Possible causes | Possible solutions |
| Change in airflow and sensation. Consider response may be to airflow, especially if patient has been without airflow to the upper airway for an extended time. | With cuff deflation: Pause in cuff deflation, allowing patient to adjust to airflow. Be sure to use very slow cuff deflation. If coughing does not subside, reinflate cuff and do not use a speaking Valve. Reintroduce slow cuff deflation after coughing subsides. With use of Valve:Remove the Valve. Allow the cough to subside. Replace the Valve. Consider short wear-times to gradually introduce patient to the upper airway airflow. |
| Secretion management. | Remove the Valve. Suction as needed. |
| Tracheostomy tube positioning. | Check the tracheostomy tube alignment and ensure tracheostomy is at midline and positioned in tract appropriately. |
| Patient positioning. | Be sure patient is sitting upright (or semi-fowler’s) with head and neck at midline. |
| Back pressure. | Remove the Valve and troubleshoot backpressure issues (see backpressure solutions under problem seven). |
| Anxiety. | Provide reassurance and education. Work on controlled exhalations through the upper airway and relaxation techniques. Involve family in the sessions. Consult clergy, social work, childlife, recreation therapy, or other appropriate personnel. |
| Coughing persists. | Consider ENT referral. |
Problem three:
The PMV is making a “honking” sound.
| Possible causes | Possible solutions |
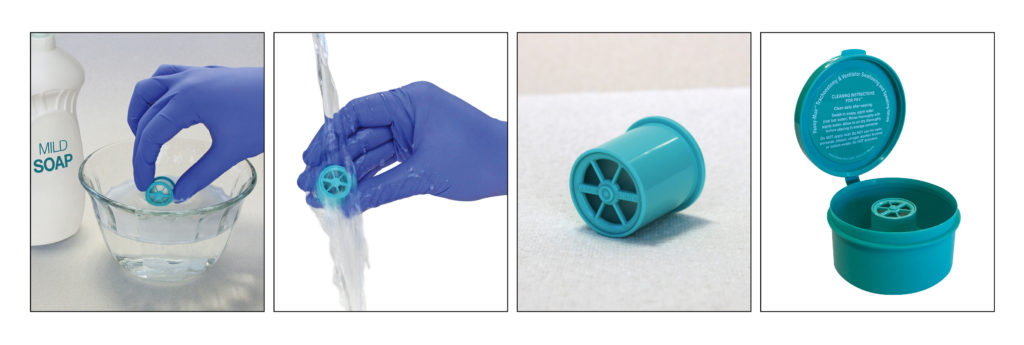
| The Valve is dirty. | The Valve should be cleaned daily as follows: Swish in warm, soapy water (use a mild soap without fragrance or lotion). Rinse under running water. Shake off and allow PMV to air dry. |
| Turbulent airflow. | Work on controlled exhalation through the upper airway. Avoid pursed lip breathing or other techniques that build pressure. |
| The Valve needs to be replaced. | The Valve lifetime is approximately two months with proper care and cleaning. If the Valve has been properly cleaned and is older than two months, consider replacing the PMV. |
Problem four:
The patient has a patent airway and is stable and comfortable with Valve use but exhibits aphonia or weak, breathy phonation.
| Possible causes | Possible solutions |
| Poor breath support. | Implement Respiratory Muscle Training (RMT) and exercises to increase breath support. |
| Laryngeal weakness. | Implement Expiratory Muscle Training (EMT) and laryngeal adduction exercises. |
| Vocal fold dysfunction or injury. | Consider ENT referral. |
| Body alignment/positioning. | Sit patient as upright as possible to enhance diaphragmatic support. |
Problem five:
Air is leaking around the stoma during PMV use.
| Possible causes | Possible solutions |
| Stoma size or wound breakdown. | Notify RN and MD for stoma care management. |
| Tracheostomy tube was downsized, and air is leaking through the stoma. | Consider use of silicone stoma pad or hydrophilic foam dressing. |
Problem six:
The patient has a patent airway but is having difficulty maintaining adequate oxygen saturation.
| Possible causes | Possible solutions |
| Cuff deflation. | 0xygen saturation may drop slightly after cuff deflation and PMV placement. Work with patient on relaxation and deep breathing techniques. |
| Inadequate breathing. | Cue patient to take deep breaths. |
| Anxiety. | Provide relaxation guidance and cue to take deep breaths. |
| Oxygen supplementation not placed. | Be sure trach collar is in place and positioned properly. Check if a nasal cannula is appropriate for use while Valve is on patient. |
| Inadequate oxygen support. | Remove Valve. Reinflate cuff. Discuss with medical team. RT may consider increasing supplemental 02 during cuff deflation and PMV use. |
Problem seven:
Back pressure (sounds like a whoosh of air) is released from the tracheostomy tube hub when the Valve is removed.
| Possible causes | Possible solutions |
| Positioning. | Reposition the patient in an upright, comfortable position with head and neck at midline. Ensure good tracheostomy tube position at midline. |
| Tracheostomy tube cuff. | Check for complete cuff deflation. |
| Tracheostomy tube. | Consider measuring transtracheal pressure with manometry to evaluate airway patency. If needed, consider downsize of tracheostomy tube. |
| Upper airway obstruction. | Consider patient history and possibility for edema; thick, copious secretions; vocal fold injury or paralysis in the adducted position; upper airway tumor; tracheal stenosis; or tracheomalacia, among others. Consider referral to ENT for assessment. |
Problem eight:
Difficulty with placement of the PMV during mechanical ventilation.
| Possible causes | Possible solutions |
| Low number of appropriate referrals. | Establish a tracheostomy order set, which includes referrals to speech-language pathology for speaking valve evaluation and use. |
| Not working as a team. | In-line PMV placement requires teamwork between the SLP and RT. |
| Inadequate knowledge and skills, low competency. | Learning opportunities for SLPs, respiratory therapists, and nurses: Ventilator Application webinars; Remote live in-services. Ventilator adjustment considerations with PMV use: https://www.passy-muir.com/vent_adjust/; Accessory and connection guide: https://www.passy-muir.com/wp-content/uploads/2018/11/connectionaccessguide1.pdf |
| Resistance from medical staff. | Provide research about the positive benefits of Valve use: https://www.passy-muir.com/wp-content/uploads/2019/01/Bibliography_2019.pdf Provide information about patients’ right to communicate, as mandated by The Americans with Disabilities Act (ADA) and The Joint Commission regulations: www.passymuir.com/resources |
Troubleshooting requires a strong knowledge base combined with critical thinking and individualized decision-making. Having a multi- or interdisciplinary team approach has shown best outcomes for patients with tracheostomies (Mah et al., 2016; Santos et al., 2018; Speed & Harding, 2013; Welton et al., 2016). Often, consultation with the medical team and other healthcare professionals is key to improving success rates. When the SLP encounters issues with PMV placement, the best approach is to determine the cause of the problem and then work toward a practical solution. Many patients can achieve successful use of the PMV both on and off mechanical ventilation. Having an SLP skilled in advocacy, intervention, and troubleshooting is key.
*This is a sponsored post from Passy-Muir.
References
Mah, J. W., Staff, I. I., Fisher, S. R., & Butler, K. L. (2016). Improving decannulation and swallowing function: A comprehensive, multidisciplinary approach to post- tracheostomy care. Respiratory Care, 62(2), 137-143.
Santos, A., Harper, D., Gandy, S., & Buchanan, B. (2018). The positive impact of multidisciplinary tracheostomy team in the care of post-tracheostomy patients. Critical Care Medicine, 46(1), 1214.
Speed, L., & Harding, K. E. (2013). Tracheostomy teams reduce total tracheostomy time and increasespeaking valve use: A systematic review and meta-analysis. Journal of Critical Care, 28(2), 216.e1-10.
Welton, C., Morrison, M., Catalig, M., Chris, J., & Pataki, J. (2016). Can an interprofessional tracheostomy team improve weaning to decannulation times? A quality improvement evaluation. Canadian Journal of Respiratory Therapy, 52 (1), 7-11.





