VitalStim: Analysis of NMES and dysphagia literature
The use of VitalStim in dysphagia therapy remains a topic of hot debate. After being used by speech pathologists for over 10 years now, you’d think the controversy would have been settled once and for all. But it seems that the more this treatment is researched the more questions are raised.
First a little VitalStim 101
VitalStim is a type of electrical stimulation (e-stim) that can stimulate the motor neurons of a muscle and facilitate a muscle contraction during functional exercise. Specifically, VitalStim is Neuromuscular Electrical Stimulation (NMES), and “VitalStim” is just a brand name, like Kleenex. NMES has been used for years by physical therapists to recruit additional muscle fibers during exercise in an effort to shorten rehabilitation time (Hainaut & Duchateau, 1992). So VitalStim is a tool that can be added to dysphagia therapy exercises, but it is not a stand-alone treatment. As with any therapy tool, it is appropriate for some patients but not others, and it is not a panacea that will work with all patients. Clinicians must apply critical reasoning skills in deciding when to use VitalStim.
Part of any good treatment decision involves consideration of Evidenced Based Practice (EBP), which includes reading the research. There’s a lot that can be debated regarding EBP with regard to VitalStim, and it is often said that there is not sufficient research about this treatment tool. Yes, there are still unanswered questions about VitalStim, but more and more studies are published on this topic every year. Fact is, more research will always be indicated for whatever we do in therapy, and our decisions in treatment boil down to “what do we know today from the research for the patients that are currently on our caseloads?” We make the best clinical decisions possible using the information that is available. When considering NMES, that means rolling up our sleeves and reading the research for ourselves.
Each research study will present conclusions but, when different studies reach different conclusions, how do we as clinicians know what to believe? In grad school, most of us learned the usual quality measures related to research studies, including study decision, potential for bias, etc.. When reviewing the research on VitalStim there are several additional factors an informed clinician will keep in mind.
When reading a study about NMES, here are some of the factors to consider:
- Remember that VitalStim is a tool that is added to traditional therapy, and we really want to know if the addition of e-stim to traditional therapy makes a significant difference. The ideal study design to see if e-stim makes a difference is the comparison of groups of patients that receive identical swallowing therapy with one group having NMES added to their therapy.
Research consideration: Randomized controlled trials (RCTs) are the best design to answer “does the addition of NMES make a statistically significant impact on dysphagia treatment?”
- NMES boosts recruitment of muscle fibers, and during NMES the patient must actively use the stimulated muscles. That’s why NMES is combined with traditional therapy. VitalStim stimulates the suprahyoid and infrahyoid muscles during dysphagia treatment, so the concurrent activity during VitalStim must use those muscles.
Research consideration: In reviewing a study, pay attention to what the patients did while the e-stim was applied. You’ll see that “traditional therapy” has very little consistency from study to study which speaks to the lack of consistency in what we do with our dysphagia patients in general. With studies looking at VitalStim, if the patients do not actively use the supra- and infrahyoid muscles, it is highly unlikely that the e-stim would have any impact on their swallowing function. For example, one study described traditional therapy as oral exercises, diet modifications, and compensatory strategies (Heijnen et al, 2012). I would not expect the addition of e-stim to make any difference in pharyngeal swallowing function when used during those therapy techniques.
- Not all e-stim is neuromuscular electrical stimulation (NMES), and not all NMES is the same electrical “formula” as VitalStim. To elaborate on this further would take us beyond the scope of this post, so let’s just leave it at “not all e-stim is the same”.
The placement of the electrodes determines which muscles are stimulated during the treatment. The placements used with the VitalStim device stimulate the suprahyoids and the thyrohyoid. Different muscles can be stimulated by changing the placement of the electrodes.
Research consideration: Do the authors use the same type of electrical stimulation and the same electrode configuration as what I’m using? Is it the same as what other studies used?
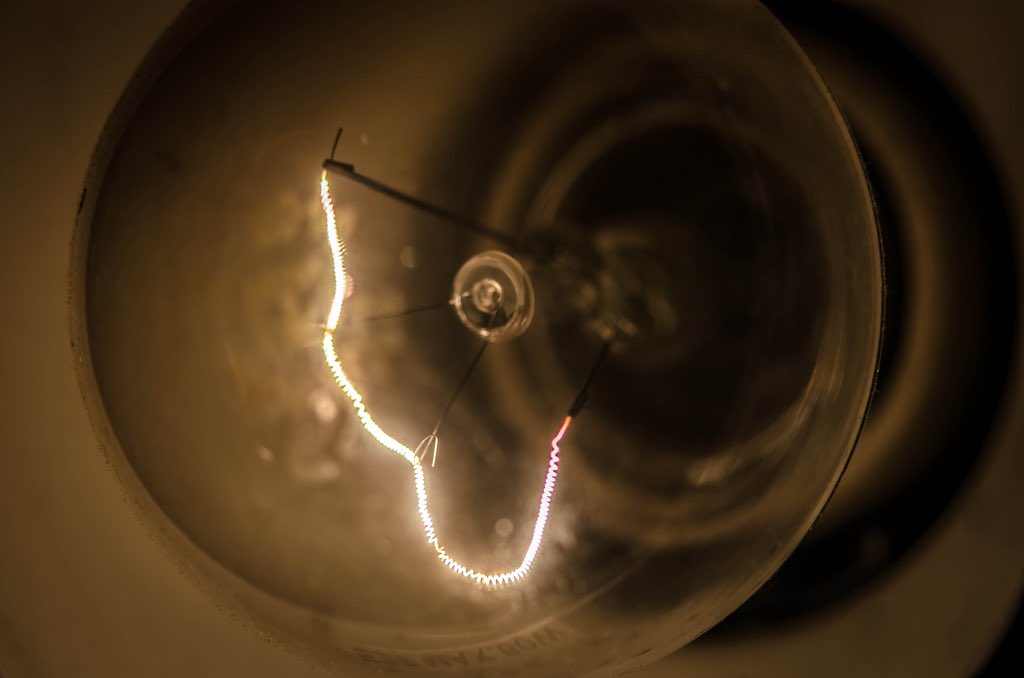
- Different nerves are stimulated by increasing the intensity of the electrical stimulation. At the lower levels, the electrical current will stimulate just the afferent nerves (sensory nerves). The patient will feel the electrical stimulation but no muscles are contracting. This level is not considered therapeutic.
As the intensity increases, some of the efferent nerves (motor nerves) that contract the muscle fibers will be stimulated. When some but not all of the muscle fibers are stimulated this is called a “sub-maximum contraction” which is ideal for treatment. At this level a patient will display signs of therapeutic intensity such as feeling a grabbing sensation of the muscles contracting slightly. If the e-stim is turned up very high, more muscle fibers will contract and the muscle can be contracted so tightly that it cannot move. This is called a “maximum contraction” and is not considered to be therapeutic as it can depress the hyoid during swallowing. This is often achieved when the e-stim is turned up as high as the patient can tolerate.
Research consideration: Do the authors specify how the intensity of the electrical stimulation used during therapy was determined? If not, the intensity level may have been too low or too high to be therapeutic.
Digging into the latest research
There are a lot of published studies looking at the use of VitalStim. In fact, there are more studies about NMES and dysphagia than just about anything we do in swallowing therapy. But we still don’t have THE answer to “VitalStim yea or nay?”
Tan et al published a meta-analysis in 2013 examining randomized controlled trials using NMES. There are also reportedly a few big RCTs that have been submitted for publication that we can hopefully read soon, so keep your eyes open for those too.
The purpose of this article is not to convince you one way or the other about the research about VitalStim. Rather, I hope to provide you with the questions you need to ask when you read current and future research studies so that you can form an opinion about the findings for yourself. Keep an open mind, keep updating your opinion as more information is available, and keep on reading that research!
References
- Hainaut, K., Duchateau, J. (1992). Neuromuscular Electrical Stimulation and Voluntary Exercise. Sports Med, 14, 100-13.
- Heijnen BJ, Speyer R, Baijens LW, Bogaardt HC. Neuromuscular electrical stimulation versus traditional therapy in patients with Parkinson’s disease and oropharyngeal dysphagia: effects on quality of life. Dysphagia. 2012;27(3):336- 345.
- Tan C, Liu Y, Li W, Liu J, Chen L. Transcutaneous neuromuscular electrical stimulation can improve swallowing function in patients with dysphagia caused by non-stroke diseases: a meta-analysis. J Oral Rehabil. Jun 2013;40(6):472-480.




