This content is sponsored by Passy-Muir
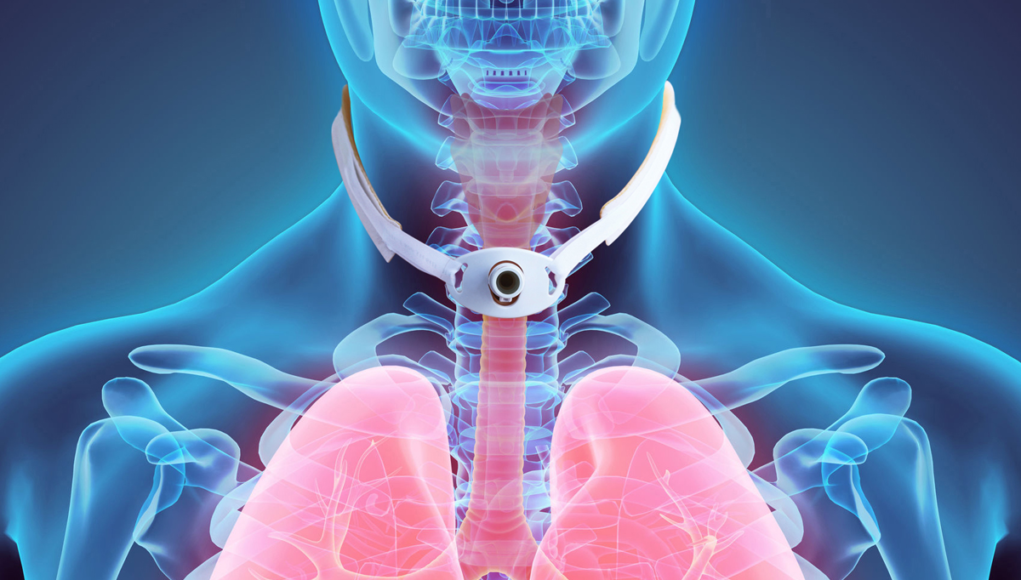
One of the goals set by the medical team for most patients with tracheostomies is to have the tracheostomy tube removed once it is no longer needed. The criteria for determining when to remove the tracheostomy tube (decannulate) is often practitioner driven and “individualized rather than protocolized” which leads to a lot of variation in practice (Singh et al., 2017). Although the criteria for considering decannulation may vary, there is one absolute criterion that must be met prior to removal of the tracheostomy tube. To safely decannulate a patient with a tracheostomy, the airway above the tracheotomy tube must be patent, with no obstruction to inspiratory or expiratory airflow through the airway. There are several methods to consider when assessing adequate airflow through the upper airway that may be used to predict successful tracheostomy tube weaning and decannulation.
Decannulation
To determine appropriateness for decannulation, it is common practice to use digital (finger) occlusion, speaking valves, or capping of the tracheostomy tube for a prescribed period of time to slowly wean from the tracheostomy tube prior to decannulation. All these practices require cuff deflation and most often require either a cuffless tracheostomy tube or a smaller sized tracheostomy tube. In addition, adequate airflow through the upper airway should be assessed early during the patient’s hospital course, even if the patient requires mechanical ventilation. Identifying issues with the upper airway early allows for the care plan to be adjusted in a timely manner to address possible issues, especially when decannulation is the ultimate goal.
The decannulation plan should begin with appropriate cuff management as soon as the artificial airway [tracheostomy tube] is inserted. When an inflated cuff is required, which occurs most often when the patient is receiving mechanical ventilation, it is important to manage the cuff appropriately to reduce the risk of late complications which may be caused by over-inflated cuffs or cuff movement. Late complications may lead to an unnecessary long-term tracheostomy (Epstein, 2005). It is suggested that cuff pressures be maintained between 15 -22 mm Hg (20 – 30 cm H2O), since capillary refill pressure normally varies between 18 and 26 mmHg, to minimize risks of tracheal wall injury and silent aspiration (Hess 2005; von Haaren et al. 2016; Kumar et al., 2020). Research has shown that a cuff pressure below 20 cmH2O is affiliated with a four times higher rate of VAP (ventilator-associated pneumonia) and cuff pressures higher than 30 cmH2O cause a higher rate of ischemic injury and possible long-term complications, such as tracheal stenosis (Kumar et al., 2020). With the risks associated with improper cuff management, it is important to monitor cuff pressures frequently to assure proper pressures are maintained.
Cuff pressures may be managed with manometry, minimal leak technique, or minimal occlusive volume technique, the most accurate of the methods (Feng et al., 2015). Minimal leak technique and minimal occlusive volume procedures to assess cuff pressures are both performed easily using a syringe and stethoscope to assess airflow in the airway either over the suprasternal notch or lateral neck; however, the preferred method is the use of a pressure manometer (Epstein, 2005; Hess, 2005; Feng et al., 2015) Although the frequency of cuff measurements is not well established, one study by Beccarria et al. (2017) reported that cuff pressures changed frequently following certain patient care procedures, most notable following bathing, which suggests that cuff pressures should be measured several times per shift.
If clinicians consider the prospect of decannulation from the time of the tracheotomy, then cuff deflation sessions may be used to assess airway patency. These sessions also would periodically restore airflow to the upper airway which may assist with diminishing the negative impact on physiologic function which may be associated with decreased use of the upper airway (King & Harrell, 2019). So, the question becomes, when is it a good time to consider cuff deflation and how do we know? Lee et al, (2016) suggested nine criteria to predict successful cuff deflation, on the first attempt. The criteria included:
- 1. medical stability
- 2. respiratory stability
- 3. fraction of inspired oxygen ≤ 0.4
- 4. tracheal suction ≤ 1-2 hourly
- 5. sputum thin and easy to suction
- 6. sputum clear or white
- 7. ≥moderate cough strength
- 8. above cuff secretions ≤ 1ml per hour
- 9. alertness – eyes open to voice
Lee reported that 95% of the patients studied were able to achieve successful cuff deflation on the first attempt. While this set of clinical considerations were used to predict successful cuff deflation in patients who were not ventilated, the same criteria could be used to consider cuff deflation sessions with patients who also require mechanical ventilation to assess upper airway patency and possible placement of a speaking valve as part of the decannulation pathway.
As a part of the cuff management process and care plan for decannulation, patency of the airway must be assessed. Several methods for assessing airway patency exist, and they vary depending on if a patient is ventilated or not. A part of the airway assessment is to deflate the cuff, allowing airflow up through the upper airway.
Airway Assessment
Cuff deflation and airway assessment for adequate airflow is straightforward when evaluating an adult patient with a tracheostomy who is not mechanically ventilated. A common practice is to deflate the cuff completely, if present, and then use finger occlusion of the tracheostomy tube during exhalation and to ask the person to speak or cough (for details of this process see King (2020)).
Clinicians make decisions which may impact the road to decannulation based on their observations of voice quality and the subjective statements made by the patient. While getting the cuff deflated is a step down the road, placing a speaking valve as part of the care plan is a further step toward decannulation.
If the airway does not appear patent or a speaking valve cannot be used, these findings may also suggest the need for tracheostomy tube downsizing or an ENT consultation to observe the airway above the tracheostomy tube. This assessment will evaluate and rule in or out any physiologic reasons for lack of airflow via the upper airway. Once the cuff of the tracheostomy tube is successfully deflated, airway patency is confirmed, and the patient is able to maintain adequate oxygenation without signs or symptoms of increased work of breathing, then continuous cuff deflation or change to a cuffless tracheostomy tube should be discussed by the team. To determine a safe decision to decannulate involves proper assessment and management of speaking valve use, capping, and secretion management. Often, the speech-language pathologist will evaluate and intervene for swallowing considerations during this process, also.
Other strategies will need to be considered when assessing infants, toddlers, non-verbal adults, or patients who require mechanical ventilation. One option is to use transtracheal pressure measurements (TTP) (for full review and description see Brooks (2018) and King (2020)). This method uses a manometer with either digital occlusion or a speaking valve to determine an objective measurement that may be used to predict airway patency. Johnson et al. (2009) used this TTP procedure on 100 spontaneously breathing patients to assess speaking valve or capping tolerance or the need to downsize the tracheostomy tube. He further indicated that use of this objective measurement led to expedited decannulation. This objective measurement may be performed on both adult and pediatric patients who are not on a ventilator; as well as those who are.
When using TTP measurements, several factors should be considered. First, complete cuff deflation must be achieved to use the TTP measurement for airway assessment. Second, if the patient is receiving mechanical ventilation, the set PEEP should be considered as part of the total TTP measurement. A more accurate reading of TTP may be observed with the set PEEP turned down or off during the measurement. It is important that the TTP measurement is taken at the end of exhalation and when the patient is in a resting breathing pattern. Crying, coughing, or voicing will increase the measurement readings since all of these conditions increase measured expiratory pressure and flow in the airway.
Mechanical Ventilation
When the patient requires mechanical ventilation, a first step on the road to decannulation is to work towards the patient using their upper airway. Airway patency may be predicted by observing inspiratory pressures and exhaled volumes measured in both the cuff inflated and deflated conditions.
Volume Ventilation
In positive pressure volume ventilation, when the cuff is inflated, the volume that is delivered from the ventilator to the patient is returned to the ventilator on exhalation and displayed as exhaled tidal volume (VTe) expressed in ml. Peak inspiratory pressure (PIP) is defined as the highest level of pressure applied to the lungs during inspiration and is expressed in cmH2O. In other words, as the volume is delivered to the lungs by the ventilator, the pressure inside the lungs increases. As the patient exhales, and the volume in the lungs decreases, the pressure inside the lungs decreases. During cuff deflation, volume delivered by the ventilator may leak during inspiration or be exhaled past the tracheostomy tube and out through the upper airway. This leak may result in decreased pressure being measured at the peak of inspiration. The volume of air that is escaping via the upper airway is not returned to the ventilator, which results in a decreased measurement of VTe. Observing a change in PIP and VTe by approximately 40-50% when the cuff is deflated may predict airway patency (Sudderth, 2016). If the airway assessment is performed when considering the use of a speaking valve, steps should be taken to assure adequate ventilation by queuing the patient to synchronize inspiratory effort with the volume breath delivery from the ventilation to assure adequate ventilation following speaking valve placement. This can be assessed by monitoring the PIP. It should be noted that the patient should be awake, alert, and meet certain criteria regarding oxygen and PEEP requirements, including a stable respiratory status. When the speech-language pathologist is assessing a patient who requires mechanical ventilation, teaming up with the respiratory therapist to suggest and adjust the ventilator may facilitate success.
Pressure Ventilation
Steps for assessing airway patency while the patient receives pressure ventilation, for example pressure control or pressure support, is similar to that of volume ventilation, except that PIP will remain a constant in pressure modes. However, the change in VTe measurement when the cuff is deflated assists with identifying a leak. Another option is to use auscultation of airflow through the upper airway to assess airway patency. As with volume ventilation, some ventilator adjustments may be required to maintain ventilation and patient comfort.
The interdisciplinary team approach, beginning with attention to proper cuff management and decision-making regarding cuff deflation and airway patency assessment, are important first steps to successful decannulation. Several methods of predicting upper airway patency are available to clinicians and early cuff deflation sessions, even with mechanical ventilation, may facilitate decannulation. Early intervention to address structural or physiologic patency issues or to identify when downsizing the tracheostomy tube should occur helps ready the patient for eventual decannulation.
*This is a sponsored post from Passy-Muir.
References
Beccaria, L.M., Doimo, T.M.A., Polletracheostomy tubei,N.A.A., Barbosa, T.P., Silva, D.C., & Werneck, A.L. (2017). Tracheal cuff pressure change before and after the performance of nursing care. Revista Brasileira de Enfermagem, 70(6),1145-50. https://doi.org/10.1590/0034-7167-2016-0486
Epstien, S.K. (2005). Late complications of tracheostomy. Respiratory Care, 50(4), 542–549.
Feng, T.R., Ye, Y., & Doyle, D.J. (2015). Clinical importance o tracheal tube cuff pressure management. World Journal of Anesthesiology, 4(2), 10 – 12. https://doi.org/ 10.5313/wja.v4.i2.10
Hess, D.R. (2005). Trachesotomy tubes and related appliances. Respiratory Care, 50(4), 497–510.
Johnson, D.C., Campbell, S.L., & Rabkin, J.D. (2009). Tracheostomy tube manometry: evaluation of speaking valves, capping and need for downsizing. The Clinical Respiratory Journal, 3(1), 8–14. https://doi.org/ 10.1111/j.1752-699X.2008.00100.x
King, K. & Harrell, M. (2019). Tracheostomy tube cuff considerations: Impact, management, and purpose. Dysphagia Café. Retrieved from https://dysphagiacafe.com/2019/10/14/tracheostomy-tube-cuff-considerations-impact-management-and-purpose/
King, K. (2020). Airway patency: What, when, how, and why. Dysphagia Café. Retrieved from https://dysphagiacafe.com/2020/11/29/airway-patency/
Kumar, C.M., Seeet, E., & Van Zundart, T.C.R.V. (2020). Measuring endotracheal tube intracuff pressure: no room for complacency. Journal of Clinical Monitoring and Computing. https://doi.org/10.1007/s10877-020-00501-2
Pryor, L. N., Ward, E. C., Cornwell, P. L., O’Connor, S. N., & Chapman, M. J. (2016). Clinical indicators associated with successful tracheostomy cuff deflation. Australia Critical Care, 29(3),132-7. https://doi.org/10.1016/j.aucc.2016.01.002
Singh, R, K., Saran, S. , Baronia, A. K. (2017). The practice of tracheostomy decannulation—a systematic review. Journal of Intensive Care, 5, 38. https://doi.org/10.1186/s40560-017-0234-z
Sudderth, G. (2016). Speaking valve use during mechanical ventilation: More than just for communication and swallowing. Talk Muir. Retrieved from https://www.passy-muir.com/talkmuir-6-1-mechanical-vent/
Von Haaren, J., Smit, J., Verhulst, M., & Vlaskamp, L. (2016). Influence of endotracheal cuff pressure on tracheal microcirculation in intubated critically ill patients. Radboudumc.