Implementing the International Dysphagia Diet Standardization Initiative (IDDSI) criteria to all the menus in facility care is a daunting task. It is also serving as an eye opener for many speech-language pathologists and dietitians. For example, soft scrambled eggs, that may have previously been included on a puree menu at some facilities are now being re-categorized more appropriately to a higher level. Although many facilities are still in the process of organizing for this effort, what we have seen is that time and space is being created in busy schedules by a dedicated team of SLPs, RDs, RNs, and food prep staff. As a result, positive change is happening to ultimately improve safety in food selection for patients. By identifying the least restrictive foods for a patient, we are also liberalizing the diet and improving chances of patient food acceptance and enjoyment. These practices are directly in line with the culture change movement happening across institutional settings, including the “New Dining Practice Standards” that recommend an individualized nutrition approach along with diet liberalization for improve quality of life (Pioneer Network, 2011).
Limited Choices in IDDSI level 6 and 5
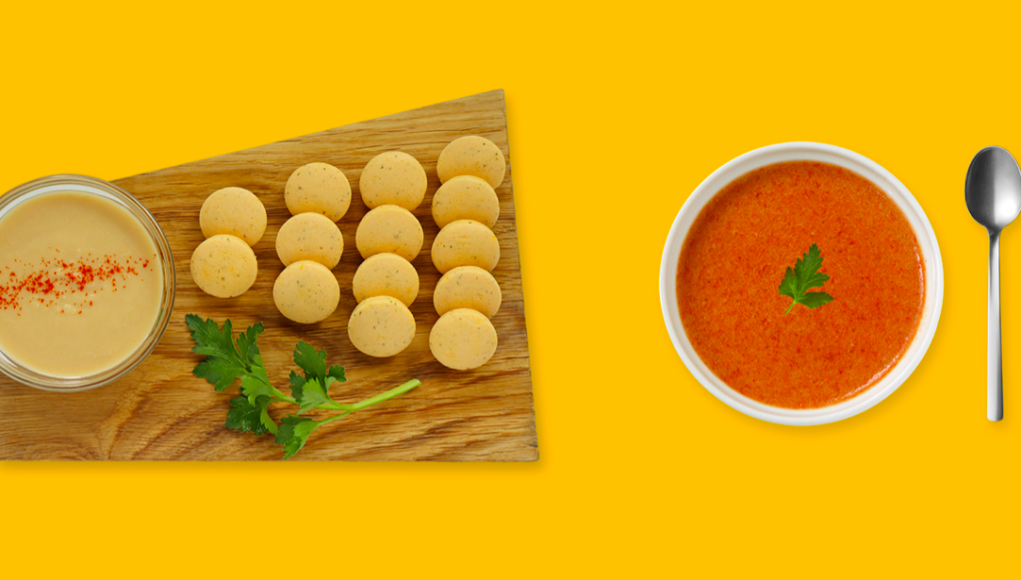
Unfortunately, there is growing concern among clinicians for the lack of choices particularly in IDDSI level 6, and 5. The lack of readily available food options fitting these levels have resulted in facilities either needing to modify current recipes or explore new ready-made food options that have not previously been used. Yet, these options are limited. Transitional foods, currently underutilized in the adult population, can offer an added option in the IDDSI levels 6 to 4 range and should be further evaluated. Transitional foods start as one texture, but change into another given the addition of moisture (water or saliva) or temperature change (Cichero et al., 2017). No biting and/or minimal chewing is required. For example, they can start as a regular or easy to chew food and transition in the mouth given the presence of saliva to puree. The historic therapeutic purpose of transitional-like solids has been as a training food in the pediatric dysphagia population or for children with underdeveloped sensorimotor systems for mastication (Dovey, 2013; Gisel, 1991). They may hold similar promise in the adult population.
Transitional foods holds great potential value for our adult patient base including:
- Rehabilitation – training food
- Screening assessments
- Increase choices in level 6,5, and potentially 4
- Improvements in self-eating skills
- Improve acceptance of a texture-modified diet
- Meet diet liberalization goals
Our emotional connection to our food
Beyond the therapy benefits for treatment and assessment, transitional foods can help with texture boredom in adult dysphagia. The closer a food in a texture-modified diet mimics the foods enjoyed in an individual’s past, the less of a deficit there is likely to be in quality of life. That can be a key purpose of transitional finger foods for adults. They can not only conjure up memories of an enjoyable snacking experience, but also encourage grazing behaviors, communal eating, and ultimately reduce risk of unwanted weight loss.
Are all transitional Foods Created Equal?
“First finger foods” are essentially a transitional food marketed to parents of toddlers as a rapid melt food to transition a child from puree to chewable solid foods. Notably, though, a study performed on these foods indicated that there was a significant amount of variability in these foods, with only a small portion meeting the safety criteria specified by the American Academy of Pediatrics (Awadalla et al., 2018). As this category gains traction in the adult population, it also remains unclear how the definition of transitional foods should be operationalized, particularly among the growing number of commercially available products, and the impact the resulting definition will have on patient safety.
The behavior of transitional foods may be drastically different across products and across patients. This can be most evident in solid foam transitional foods such as Savoreaseô crackers, shrimp chips, Cheeto Puffsô, wafer cookies, and the EAT barô. The predominant reason is the amount of saliva present to initiate the dissolution of these foods. Saliva is a biofluid composed predominantly of water, but also contains various electrolytes, small organic substances, proteins, peptides and polynucleotides. It functions to aid not only in lubrication, but also in initiating digestion of foods. Although the IDDSI testing method involves the placement of a 1.5 cm x 1.5 cm piece of food in 1 cc of water for 1 minute, many individuals do not have 1 cc of saliva present in their mouths at a given time, saliva differs in composition from water alone, and 1 minute exceeds the typical oral transit times (OTT) of food through the oral cavity (1-12.8 seconds (Soares et al., 2015). Further, even if transitional foods meet the IDDSI criteria based on the specified benchtop testing methods, it is not known how they will behave in an individual with dysphagia, with or without potential underlying xerostomia.
We recently conducted a study to examine this issue (Barewal et al., 2019). The dissolution of a variety of commercially available foods was tested using standard IDDSI testing methods and multiple oral conditions (5 and 12 seconds in the oral cavity with and without lingual pressure). It was found that although most of the foods that were tested dissolved adequately following standard IDDSI testing, product dissolution in the mouth measured after 5 and 12 seconds in individuals with or without dry mouth was quite variable.
Transitional Foods: A Potential Benefit for your Patients
The potential benefits of including transitional foods in the diet of individuals with dysphagia are widespread, including improved nutritional intake and quality of life. Thus, it is clearly a worthwhile endeavor to explore this category with our patients. However, we encourage testing of transitional foods not only with IDDSI measures, but also during assessments to determine individual appropriateness. We also support continued research into the properties and oral processing of transitional-state foods in order to further integrate this food category into standard clinical practice.
Links of Interest
References
- Pioneer Network (2011). New dining practice standards. Food and Dining Clinical Standards Task Force. https://www.pioneernetwork.net/Data/Documents/NewDiningPracticeStandards.pdf
- Cichero et al. Dysphagia. 2017. doi:10.1007/y
- Dovey et al. Dysphagia. 2013.doi.org/10.1007/s00455-013-9460-2
- Gisel. Dev Med Child Neurol. 1991. doi.org/10.1111/j.1469-8749.1991.tb14786.x
- Awadalla et al. Clinical Pediatrics. 2018. doi.org/10.1177/0009922817733701
- Soares et al. Arg Bras Cir Dig. 2015. doi.org/10.1590/s0102-67202015000200015
- Barewal, R. & Shune, S. (2019). The oral dissolution rate of transitional snack foods in adults with and without dry mouth [abstract]. Journal of the Academy of Nutrition and Dietetics, 119(10), A115.
Co-Author Biography: Samantha Shune, PhD, CCC-SLP is an assistant professor in Communication Disorders and Sciences and research scientist in the Prevention Science Institute at the University of Oregon. Her research program is aimed at mitigating the deleterious effects of both healthy and pathologic aging on the eating process. Drawing on her clinical background in medical speech-language pathology, she is focused on integrating the physiologic components of swallowing with a more holistic view of the mealtime process (e.g., cognition, communication, socialization/social relationships). She is particularly interested in how the translation of such research into clinical practice can promote both mealtime safety and improved quality of life for patients and their families across the lifespan.
Disclosure for Dr. Shune: Dr. Shune has an ongoing volunteer advisory relationship with the founder of Savorease Therapeutic Snacks (Taste for Life, LLC).
Disclosure for Dr. Barewal: Research materials for this study were partially funded by Taste For Life, LLC, a company owned by Dr. Barewal. The mission of Taste For Life is to meet the needs of everyone on a restricted diet through compassion, research and education.