Co-Authors: Catriona M. Steele, Ph.D., CCC-SLP, S-LP(C), Reg. CASLPO, ASHA Fellow & Julie Peterson, MS, CCC-SLP
With standardization on the forefront of current healthcare practices, the Modified Barium Swallow Impairment Profile (MBSImP™), VARIBAR® barium sulfate (Bracco Diagnostics Inc.), and the International Dysphagia Diet Standardisation Initiative (IDDSI) are widely recognized as initiatives that promote standardization in dysphagia evaluation and treatment. As individuals who have been involved in the development and implementation of these initiatives, each of us receives inquiries as to how they relate to one another. We felt it was important to address these queries in this collaborative comment.
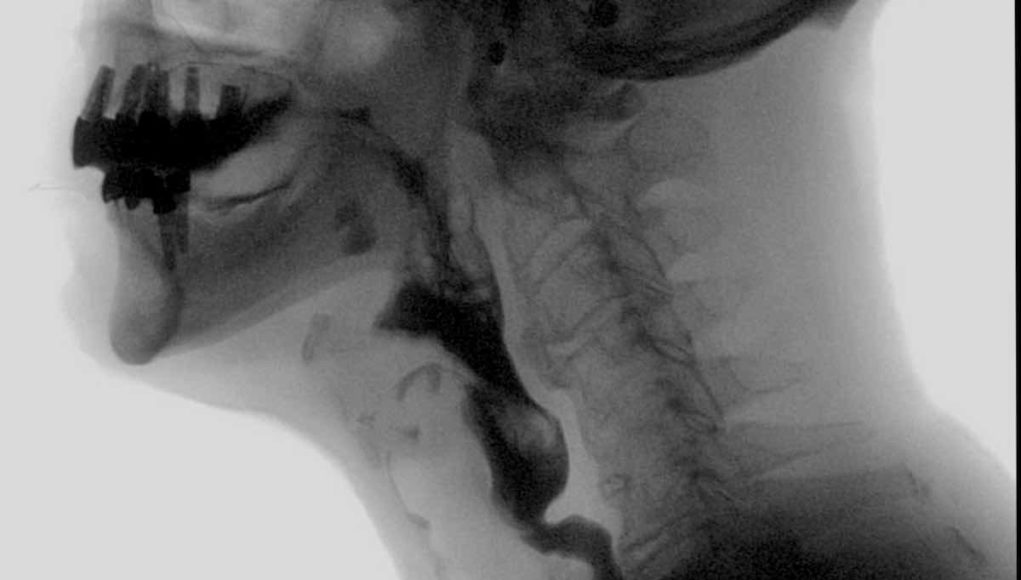
Accurate diagnostic information attained from the Modified Barium Swallow Study (MBSS), when paired with other clinical evaluations, patient history and clinician judgment, provides the basis for determining a patient’s physiologic swallowing diagnosis.
A risk/benefit analysis must be made by the clinician related to patient safety in terms of aspiration events as well as patient and clinician safety related to radiation exposure. A standard protocol, using standardized stimuli, is recommended for answering medically important questions efficiently while limiting unnecessary radiation exposure.
Decisions to explore interventions or items beyond a standard protocol must always be made in the context of the purpose of the exam, balancing diagnostic yield with patient and operator safety and efficiency.
Purpose of MBSS
- Identify and distinguish the presence, type and estimated severity of physiologic swallowing impairment
- Determine the safety of oral intake (airway protection)
- Determine the efficiency of oral intake (clearance)
- Detail the effects of selected front-line interventions (postures, maneuvers, bolus variables) on swallowing physiology, airway protection and efficiency.
- Identify indications for specific interventions that are appropriate for the clinical condition of the patient
- Develop intake (oral, tube etc.) and diet texture/nutritional management plans in collaboration with the physician and interdisciplinary team.
Protocols
The MBSS should employ a protocol characterized by core elements or standards that facilitate:
- patient and clinician safety;
- reproducible examination results;
- valid observations and measures;
- patient and provider understanding and expectations regarding the procedure and expected outcomes.
Within the context of these core elements there should be flexibility for reasonable modification based on the clinical circumstances of the patient, or specific clinical questions addressed using rationally and empirically based interventions.
A standardized set of barium preparations (VARIBAR®) has been developed, currently for distribution in the US, which is FDA approved and specifically labeled for MBSS. The user should use these standardized products as is (without modification). “Off-label use”, (i.e. altering them from the manufacturer’s instructions for use) compromises the standardization goal of the product.
There are 5 primary reasons to avoid the use of modified, off-label food and liquid barium materials during MBSS:
- Aspiration of food and liquid materials other than inert barium is a threat to pulmonary health;
- Preparation of contrast materials that will be ingested needs to be compliant with food safety regulations, pharmaceutical regulations and infection control policies;
- Standardized barium products have been formulated and are factory produced with strict quality control monitoring. Off-label mixing of other barium powders or suspensions with foods and liquids may alter viability and visibility on x-ray;
- There is no guarantee that clinician-made mixtures in radiology will be replicated at the bedside. Clinicians who understand and are able to identify physiologic elements of swallowing impairment in the context of multiple patient factors (cognition, adherence, support) will be able to predict how patients will swallow with very subtle changes to consistency, or with other modifications that impact bolus flow, such as adjustments of bolus size, patient position and administration methods;
- MBSS findings should always be validated whenever possible via observation of patient performance at the bedside or at mealtime.
Use of standardized barium products ensures reproducible results across MBSS examinations. Although it is not possible for standard barium products to achieve an exact match to the nearly endless complement of consistencies that may appear in real-life foods and liquids, the VARIBAR® products are mapped to levels 0-4 (thin to extremely thick) on the IDDSI global framework for naming, describing and measuring the texture of foods and liquids (www.iddsi.org). The IDDSI naming conventions have been incorporated into the MBSImP report writing template (www.mbsimp.com), as an option for those who have adopted this initiative.
Co-Authors Biography
Catriona M. Steele, Ph.D., CCC-SLP, S-LP(C), Reg. CASLPO, ASHA Fellow
Professor Catriona M. Steele is a clinician scientist working in the area of swallowing and swallowing disorders. She has a background as a medical speech-language pathologist, and is Director of the Swallowing Rehabilitation Research Laboratory (www.steeleswallowinglab.ca) at KITE, the research arm of the Toronto Rehabilitation Institute – University Health Network. Dr. Steele is a Professor in the Department of Speech-Language Pathology at the University of Toronto.
Professor Steele holds research funding from the National Institutes of Health (USA) as well as several active industry contracts. She is an associate editor for the Dysphagia journal and a member of the editorial board for the Journal of Texture Studies. She is also a member of the Board of Directors for the International Dysphagia Diet Standardisation Initiative (www.iddsi.org).
Julie Peterson, MS, CCC-SLP
Julie Peterson received her M.S. in Speech Pathology at MSU in Moorhead, MN. She has practiced in the public schools, acute care, rehabilitation, home health and long term care. She has worked in educational publishing, software, and medical technologies. She currently serves as Senior Clinical Sales Specialist/subject matter expert and Marketing Manager for Dysphagia at Bracco Diagnostics, Oral Imaging.